Ankle Injuries: A Sprained Ankle ?
Radiology Cases in Pediatric Emergency Medicine
Volume 3, Case 3
Alson S. Inaba MD
Kapiolani Medical Center For Women And Children
University of Hawaii John A. Burns School of Medicine
A 17 year old male presents to the Emergency
Department one day after sustaining a "twisting" injury
to his left ankle while playing soccer. The patient
claims to have sustained a "twisted ankle" while he was
running towards the goal. He does not recall exactly in
which direction his ankle twisted. He did not feel or
hear any "snaps," "pops," or "clicks." Although he was
able to bear some weight on the ankle immediately after
the injury, today he has much more pain and swelling
about the anterior and lateral aspect of the affected
ankle. Overnight he did not elevate the ankle nor did he
apply any ice to the injured ankle. He denies sustaining
any other injuries and has not sustained any previous
injury to his left ankle. This morning he is unable to
walk on the ankle secondary to increased pain and
swelling.
On examination, he is barely able to bear any weight
on the affected ankle secondary to pain. There is
obvious swelling (without ecchymosis) to the anterior
and lateral aspect of the ankle joint. Distally, his toes
are pink, with brisk capillary refill and intact sensation to
light touch. Tenderness can be elicited by palpation
over the anterior aspect of the ankle joint (Refer to
photo).
Review area of tenderness.
 The black arrow points to the region of maximum
tenderness. There is no tenderness along the inferior
tip of the lateral malleolus or over the bony prominence
of the lateral malleolus. There is no tenderness along
the medial aspect of the ankle or along the proximal
aspects of both the tibial and fibular shafts. The
squeeze test over the distal tibia-fibula region does not
produce any pain. Both the anterior drawer and talar tilt
maneuvers are within normal limits when compared to
the nonaffected ankle.
Questions:
a) Has this patient sustained a typical ankle sprain?
b) What is the typical mechanism of injury for the
majority of ankle sprains sustained during sporting
events?
c) Which ankle ligament is most commonly sprained
during an inversion injury, and where on the ankle
should one palpate to check for tenderness to this
ligament?
d) Describe the anterior drawer test and what
specifically does this maneuver test for?
e) Describe the talar tilt test and what specifically
does this maneuver test for?
f) What is the syndesmosis, and how does one
examine for possible syndesmotic injuries?
Discussion & Teaching Points:
Ankle injuries are one of the most common
sports-related orthopedic injuries seen in the
Emergency Department. These types of injuries are
most commonly sustained in patients between 15 - 35
years of age. The majority of ankle sprains (up to 85%)
are due to inversion injuries while only 15% are due to
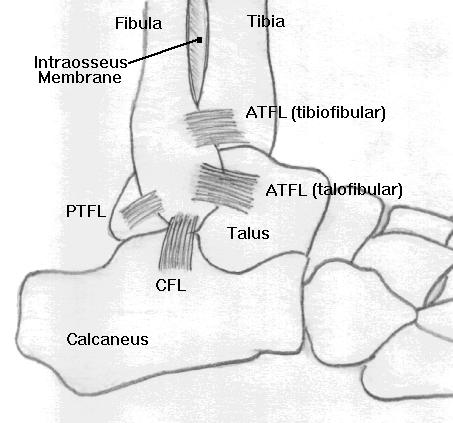
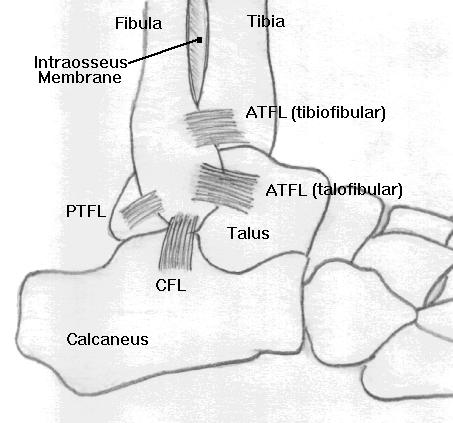
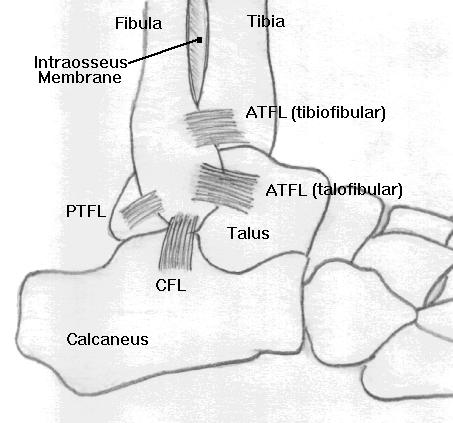
eversion-related injuries. There are 3 lateral ankle
ligaments and one broad, fan-shaped medial ligament.
Review the ligaments.
The black arrow points to the region of maximum
tenderness. There is no tenderness along the inferior
tip of the lateral malleolus or over the bony prominence
of the lateral malleolus. There is no tenderness along
the medial aspect of the ankle or along the proximal
aspects of both the tibial and fibular shafts. The
squeeze test over the distal tibia-fibula region does not
produce any pain. Both the anterior drawer and talar tilt
maneuvers are within normal limits when compared to
the nonaffected ankle.
Questions:
a) Has this patient sustained a typical ankle sprain?
b) What is the typical mechanism of injury for the
majority of ankle sprains sustained during sporting
events?
c) Which ankle ligament is most commonly sprained
during an inversion injury, and where on the ankle
should one palpate to check for tenderness to this
ligament?
d) Describe the anterior drawer test and what
specifically does this maneuver test for?
e) Describe the talar tilt test and what specifically
does this maneuver test for?
f) What is the syndesmosis, and how does one
examine for possible syndesmotic injuries?
Discussion & Teaching Points:
Ankle injuries are one of the most common
sports-related orthopedic injuries seen in the
Emergency Department. These types of injuries are
most commonly sustained in patients between 15 - 35
years of age. The majority of ankle sprains (up to 85%)
are due to inversion injuries while only 15% are due to
eversion-related injuries. There are 3 lateral ankle
ligaments and one broad, fan-shaped medial ligament.
Review the ligaments.
 Although ankle sprains are common in older
adolescent patients and young adults, isolated ankle
sprains are not very common in younger children and
in preadolescent patients. The physis (growth plate) in
these younger children is much weaker than the
surrounding ligaments, and is thus more susceptible to
injury. Therefore in the pediatric population, injuries
involving the growth plates (Salter-Harris injuries) must
also be considered in addition to ligament sprains.
The anterior talofibular ligament (ATFL) is the
weakest of the 3 lateral ligaments and is the most
commonly injured of the lateral ankle ligaments. (Note
that ATFL can also stand for anterior tibiofibular
ligament, however, in this case, ATFL will be used to
stand for anterior talofibular ligament.) 65% of lateral
ligament sprains are confined to the ATFL alone, while
20% have concomitant calcaneofibular ligament (CFL)
tears. The ATFL can be palpated just inferior and
anterior to the distal most aspect of the lateral
malleolus.
Review ATFL location.
Although ankle sprains are common in older
adolescent patients and young adults, isolated ankle
sprains are not very common in younger children and
in preadolescent patients. The physis (growth plate) in
these younger children is much weaker than the
surrounding ligaments, and is thus more susceptible to
injury. Therefore in the pediatric population, injuries
involving the growth plates (Salter-Harris injuries) must
also be considered in addition to ligament sprains.
The anterior talofibular ligament (ATFL) is the
weakest of the 3 lateral ligaments and is the most
commonly injured of the lateral ankle ligaments. (Note
that ATFL can also stand for anterior tibiofibular
ligament, however, in this case, ATFL will be used to
stand for anterior talofibular ligament.) 65% of lateral
ligament sprains are confined to the ATFL alone, while
20% have concomitant calcaneofibular ligament (CFL)
tears. The ATFL can be palpated just inferior and
anterior to the distal most aspect of the lateral
malleolus.
Review ATFL location.
 The white arrow points to the region of the ATFL.
Because the patient in this case has point tenderness in
an area other than over the ATFL, he has therefore not
sustained a typical ankle sprain. In comparison to
these lateral ligaments, the medial, deltoid ligament has
a fair degree of elasticity and is much more resistant to
tears.
Most injuries also occur while the ankle joint is in
plantar flexion rather than in dorsiflexion. Anatomically,
the talar dome is wedge-shaped, with the anterior
aspect of the talus being wider than the posterior
aspect. During dorsiflexion, this wider, anterior aspect
of the talus is engaged within the mortise (formed by
the distal tibia and fibula), and the joint is very stable.
However during plantar flexion, the narrower, posterior
aspect of the talus becomes engaged in the ankle
mortise.
Review joint space diagram.
The white arrow points to the region of the ATFL.
Because the patient in this case has point tenderness in
an area other than over the ATFL, he has therefore not
sustained a typical ankle sprain. In comparison to
these lateral ligaments, the medial, deltoid ligament has
a fair degree of elasticity and is much more resistant to
tears.
Most injuries also occur while the ankle joint is in
plantar flexion rather than in dorsiflexion. Anatomically,
the talar dome is wedge-shaped, with the anterior
aspect of the talus being wider than the posterior
aspect. During dorsiflexion, this wider, anterior aspect
of the talus is engaged within the mortise (formed by
the distal tibia and fibula), and the joint is very stable.
However during plantar flexion, the narrower, posterior
aspect of the talus becomes engaged in the ankle
mortise.
Review joint space diagram.
 Note the obvious widening of the joint space during
plantar flexion on the left compared to dorsiflexion on
the right. Thus, with this understanding of the
articulation of the talus within the mortise, it is not
surprising that most ankle injuries occur while the ankle
is in plantar flexion, rather than in dorsiflexion.
The last part of the clinical examination of an injured
ankle involves assessing the stability of the ankle joint.
The two maneuvers that can be performed to assess
the stability of the ankle joint are the anterior drawer
and talar tilt maneuvers. Keep in mind that the ability to
perform these tests and the results immediately after an
injury may be limited by swelling, pain and muscle
spasm. Do not attempt to perform either of these tests
if there is an obvious deformity of the ankle suggestive
of a possible ankle fracture.
The ATFL ligament normally prevents the anterior
subluxation of the talus from the mortise. The talus
may be subluxed anteriorly whenever the ATFL is
partially ruptured (second-degree sprain) or completely
ruptured (third-degree sprain). The anterior drawer
maneuver assesses the integrity of the ATFL. Since
the ATFL is usually the first ligament to be injured in a
typical inversion injury, some physicians feel that if this
anterior drawer test is negative, it is then unnecessary
to perform the talar tilt maneuver (since the talar tilt
stress test is positive only if both the ATFL and the CFL
are injured). To perform the anterior drawer maneuver,
the patient can either be supine or sitting down, with the
ankle in neutral position. One hand of the examiner
cups the heel of the affected ankle (and attempts to pull
the foot anteriorly), while the other hand braces along
the anterior aspect of the lower leg.
Review drawer sign maneuver.
Note the obvious widening of the joint space during
plantar flexion on the left compared to dorsiflexion on
the right. Thus, with this understanding of the
articulation of the talus within the mortise, it is not
surprising that most ankle injuries occur while the ankle
is in plantar flexion, rather than in dorsiflexion.
The last part of the clinical examination of an injured
ankle involves assessing the stability of the ankle joint.
The two maneuvers that can be performed to assess
the stability of the ankle joint are the anterior drawer
and talar tilt maneuvers. Keep in mind that the ability to
perform these tests and the results immediately after an
injury may be limited by swelling, pain and muscle
spasm. Do not attempt to perform either of these tests
if there is an obvious deformity of the ankle suggestive
of a possible ankle fracture.
The ATFL ligament normally prevents the anterior
subluxation of the talus from the mortise. The talus
may be subluxed anteriorly whenever the ATFL is
partially ruptured (second-degree sprain) or completely
ruptured (third-degree sprain). The anterior drawer
maneuver assesses the integrity of the ATFL. Since
the ATFL is usually the first ligament to be injured in a
typical inversion injury, some physicians feel that if this
anterior drawer test is negative, it is then unnecessary
to perform the talar tilt maneuver (since the talar tilt
stress test is positive only if both the ATFL and the CFL
are injured). To perform the anterior drawer maneuver,
the patient can either be supine or sitting down, with the
ankle in neutral position. One hand of the examiner
cups the heel of the affected ankle (and attempts to pull
the foot anteriorly), while the other hand braces along
the anterior aspect of the lower leg.
Review drawer sign maneuver.
 If the foot of the affected ankle can be pulled forward
by more than 3 - 5 mm (or if the affected ankle can be
subluxed more forward than the nonaffected side),
suspect a rupture of the ATFL.
The talar tilt test assesses the integrity of the CFL.
To perform this maneuver the patient can again be
either sitting down or supine, with the ankle in neutral
position. While one hand of the examiner holds the
lower leg stationary, the other hand gently attempts to
invert the ankle.
Review talar tilt maneuver.
If the foot of the affected ankle can be pulled forward
by more than 3 - 5 mm (or if the affected ankle can be
subluxed more forward than the nonaffected side),
suspect a rupture of the ATFL.
The talar tilt test assesses the integrity of the CFL.
To perform this maneuver the patient can again be
either sitting down or supine, with the ankle in neutral
position. While one hand of the examiner holds the
lower leg stationary, the other hand gently attempts to
invert the ankle.
Review talar tilt maneuver.
 Greater than 10 degrees of difference in the talar tilt
when compared to the nonaffected side is suggestive of
an injury to the CFL.
Proximal to the lateral and medial ankle ligaments,
the distal tibia and distal fibula are connected to each
other by a series of tough fibrous structures collectively
referred to as the tibiofibular syndesmosis. The three
individual components which make-up this syndesmosis
include: a) anterior tibiofibular ligament, b) posterior
tibiofibular ligament, and c) intraosseous membrane.
Review syndesmosis anatomy.
Greater than 10 degrees of difference in the talar tilt
when compared to the nonaffected side is suggestive of
an injury to the CFL.
Proximal to the lateral and medial ankle ligaments,
the distal tibia and distal fibula are connected to each
other by a series of tough fibrous structures collectively
referred to as the tibiofibular syndesmosis. The three
individual components which make-up this syndesmosis
include: a) anterior tibiofibular ligament, b) posterior
tibiofibular ligament, and c) intraosseous membrane.
Review syndesmosis anatomy.
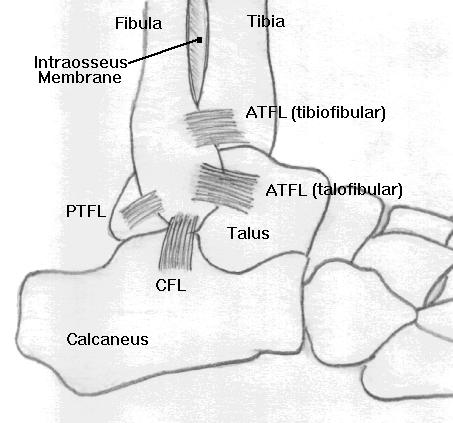 Note that on this diagram, the PTFL stands for the
posterior talofibular ligament (not the posterior
tibiofibular ligament). The posterior tibiofibular ligament
is NOT drawn on this diagramatic view.
Clinically one can check for injuries of the tibiofibular
syndesmosis by the squeeze test. To perform this test,
the examiner firmly grasps the patient's lower leg
(around the lower aspect of the calf), and gently
squeezes the tibia and fibula together.
Review squeeze test.
Note that on this diagram, the PTFL stands for the
posterior talofibular ligament (not the posterior
tibiofibular ligament). The posterior tibiofibular ligament
is NOT drawn on this diagramatic view.
Clinically one can check for injuries of the tibiofibular
syndesmosis by the squeeze test. To perform this test,
the examiner firmly grasps the patient's lower leg
(around the lower aspect of the calf), and gently
squeezes the tibia and fibula together.
Review squeeze test.
 Provided that there are no fractures of the tibial or
fibular shafts, if ankle pain can be elicited by this
squeeze maneuver, one should suspect an injury to one
or more of the components of the tibiofibular
syndesmosis.
Questions:
a) What are some clinical criteria that would warrant
a radiographic examination of an injured ankle?
b) What are the 3 standard radiographic views that
are obtained on patients with ankle injuries?
c) When do the distal tibial and distal fibular
epiphyses appear, and by what age do these epiphyses
fuse to the adjacent metaphyses?
Discussion & Teaching Points
It is estimated that over $500 million dollars are
spent each year on ankle radiographs. However the
majority (up to 85%) of these radiographs are negative.
In 1992, a Canadian study suggested the adaptation of
the Ottawa ankle rules, which could be used to order
ankle radiographs based on selected clinical criteria. It
is important to remember that this study excluded
patients younger than 18 years of age. Therefore,
since the Ottawa study did not include growth plate
injuries, one should not strictly adhere to these rules
when deciding whether or not to obtain a radiograph on
a pediatric patient. Based on these Ottawa ankle rules,
clinical indications that would warrant a radiographic
evaluation would include any one of the following
criteria:
a) Inability to bear weight both immediately after the
injury and in the Emergency Department.
b) Bony tenderness over the posterior edge, tip or
distal 6 cm of the lateral malleolus.
c) Bony tenderness over the posterior edge, tip or
distal 6 cm of the medial malleolus.
d) Tenderness over the base of the 5th metatarsal.
A complete, standard radiograph examination of the
ankle should include 3 views (AP, lateral, and a mortise
view).
Review ankle views.
Provided that there are no fractures of the tibial or
fibular shafts, if ankle pain can be elicited by this
squeeze maneuver, one should suspect an injury to one
or more of the components of the tibiofibular
syndesmosis.
Questions:
a) What are some clinical criteria that would warrant
a radiographic examination of an injured ankle?
b) What are the 3 standard radiographic views that
are obtained on patients with ankle injuries?
c) When do the distal tibial and distal fibular
epiphyses appear, and by what age do these epiphyses
fuse to the adjacent metaphyses?
Discussion & Teaching Points
It is estimated that over $500 million dollars are
spent each year on ankle radiographs. However the
majority (up to 85%) of these radiographs are negative.
In 1992, a Canadian study suggested the adaptation of
the Ottawa ankle rules, which could be used to order
ankle radiographs based on selected clinical criteria. It
is important to remember that this study excluded
patients younger than 18 years of age. Therefore,
since the Ottawa study did not include growth plate
injuries, one should not strictly adhere to these rules
when deciding whether or not to obtain a radiograph on
a pediatric patient. Based on these Ottawa ankle rules,
clinical indications that would warrant a radiographic
evaluation would include any one of the following
criteria:
a) Inability to bear weight both immediately after the
injury and in the Emergency Department.
b) Bony tenderness over the posterior edge, tip or
distal 6 cm of the lateral malleolus.
c) Bony tenderness over the posterior edge, tip or
distal 6 cm of the medial malleolus.
d) Tenderness over the base of the 5th metatarsal.
A complete, standard radiograph examination of the
ankle should include 3 views (AP, lateral, and a mortise
view).
Review ankle views.
 a) AP view: There are several findings that can be
observed on the AP view. The tip of the lateral
malleolus normally extends more distally than the tip of
the medial malleolus. The syndesmosis of the ankle
joint normally causes an overlap of the medial aspect of
the distal fibula and the lateral aspect of the distal tibia
on this AP view. Therefore, subtle fractures involving
either the lateral aspect of the distal tibia or the medial
aspect of the distal fibula (i.e., between the tibia and
fibula) may be difficult to visualize on this AP view alone
because of the overlap. It is a common pitfall to miss a
Salter Harris Type III fracture of the distal lateral tibia
because it is obscured by the overlapping fibula.
b) Lateral view: On a true lateral view, the malleoli
should be superimposed upon one another. The lateral
view provides a better view of the posterior aspect of
the distal tibia and fibula, the talus, calcaneus and the
base of the 5th metatarsal.
c) Mortise view: To obtain a better view of the
ankle mortise, the patient's leg must be internally
rotated just enough so that the lateral malleolus (which
is normally posterior to the medial malleolus), is on the
same horizontal plane as the medial malleolus, and a
line drawn through both malleoli would be parallel to the
tabletop. Usually this only requires approximately 10 -
20 degrees of internal rotation. In other words, whe
n viewing the mortise view, the tibia and fibula must be
viewed without superimposition on each other. This
mortise view represents a true AP projection of the
ankle mortise and also provides a good visualization of
the talar dome (to rule-out osteochondral talar dome
fractures). The clear joint space [formed by the
talofibular joint, the superior space between the dome
of the talus & the tibial plafond (the inferior articulating
surface of the tibia) and the tibiotalar joint] should all
uniformly measure 3 - 4 mm. A difference of greater
than 2 mm (i.e., the joint space width varies by more
than 2 mm. Eg., Joint space measures 2 mm at lateral
part of joint and 5 mm at medial side of joint.) is
suggestive of mortise instability.
If all of the above 3 views appear normal in a patient
with a high clinical suspicion of a fracture, one should
then obtain internal and external oblique views of the
ankle to obtain additional views of the distal tibia and
distal fibula. To obtain such views, the patient's leg is
rotated 45 degrees internally, then 45 degree externally.
The epiphyses of the distal tibia and fibula both
appear by 2 years of age. The physis of the distal tibia
fuses to its adjacent metaphysis by 18 years of age.
The physis of the distal fibula fuses to its adjacent
metaphysis by 20 years of age. Therefore, growth plate
injuries should still be considered as a possibility in any
patient up to 20 years of age. If one is unsure if a
radiolucent line involving the distal tibia or fibula
represents either a physis or an actual fracture,
consider obtaining a comparison view of the
nonaffected ankle.
An x-ray of the patient's ankle was obtained.
Review our patient's ankle radiographs.
a) AP view: There are several findings that can be
observed on the AP view. The tip of the lateral
malleolus normally extends more distally than the tip of
the medial malleolus. The syndesmosis of the ankle
joint normally causes an overlap of the medial aspect of
the distal fibula and the lateral aspect of the distal tibia
on this AP view. Therefore, subtle fractures involving
either the lateral aspect of the distal tibia or the medial
aspect of the distal fibula (i.e., between the tibia and
fibula) may be difficult to visualize on this AP view alone
because of the overlap. It is a common pitfall to miss a
Salter Harris Type III fracture of the distal lateral tibia
because it is obscured by the overlapping fibula.
b) Lateral view: On a true lateral view, the malleoli
should be superimposed upon one another. The lateral
view provides a better view of the posterior aspect of
the distal tibia and fibula, the talus, calcaneus and the
base of the 5th metatarsal.
c) Mortise view: To obtain a better view of the
ankle mortise, the patient's leg must be internally
rotated just enough so that the lateral malleolus (which
is normally posterior to the medial malleolus), is on the
same horizontal plane as the medial malleolus, and a
line drawn through both malleoli would be parallel to the
tabletop. Usually this only requires approximately 10 -
20 degrees of internal rotation. In other words, whe
n viewing the mortise view, the tibia and fibula must be
viewed without superimposition on each other. This
mortise view represents a true AP projection of the
ankle mortise and also provides a good visualization of
the talar dome (to rule-out osteochondral talar dome
fractures). The clear joint space [formed by the
talofibular joint, the superior space between the dome
of the talus & the tibial plafond (the inferior articulating
surface of the tibia) and the tibiotalar joint] should all
uniformly measure 3 - 4 mm. A difference of greater
than 2 mm (i.e., the joint space width varies by more
than 2 mm. Eg., Joint space measures 2 mm at lateral
part of joint and 5 mm at medial side of joint.) is
suggestive of mortise instability.
If all of the above 3 views appear normal in a patient
with a high clinical suspicion of a fracture, one should
then obtain internal and external oblique views of the
ankle to obtain additional views of the distal tibia and
distal fibula. To obtain such views, the patient's leg is
rotated 45 degrees internally, then 45 degree externally.
The epiphyses of the distal tibia and fibula both
appear by 2 years of age. The physis of the distal tibia
fuses to its adjacent metaphysis by 18 years of age.
The physis of the distal fibula fuses to its adjacent
metaphysis by 20 years of age. Therefore, growth plate
injuries should still be considered as a possibility in any
patient up to 20 years of age. If one is unsure if a
radiolucent line involving the distal tibia or fibula
represents either a physis or an actual fracture,
consider obtaining a comparison view of the
nonaffected ankle.
An x-ray of the patient's ankle was obtained.
Review our patient's ankle radiographs.
 How would you interpret these 2 views? Oblique
and mortise views were also obtained because of the
physical exam findings.
Review mortise view.
How would you interpret these 2 views? Oblique
and mortise views were also obtained because of the
physical exam findings.
Review mortise view.
 What does this mortise view reveal that may not
have be very evident on the 2 previous views?
Radiographic interpretation: There is a moderate
amount of soft tissue swelling over the lateral malleolus.
The AP and lateral views do not reveal any obvious
fractures. However, there is a subtle widening of the
medial aspect of the distal fibular growth plate (physis)
on the mortise view. Comparative views and/or stress
views would confirm that this is a fracture versus a
normal growth plate closure.
Questions:
a) Does this patient require immediate orthopedic
intervention or can he be sent home from the
Emergency Department with an out-patient orthopedic
referral?
b) If you would send this patient home, what type of
dressing or splint would you apply?
Discussion & Teaching Points:
This patient has sustained a nondisplaced
Salter-Harris type I fracture of the distal fibula (lateral
malleolus). Clinical and or radiographic criteria that
would warrant immediate orthopedic intervention
include:
a) An open fracture.
b) Any type of injury with neurovascular
compromise.
c) Any unstable fracture (which would be difficult to
adequately immobilize in a splint).
d) Any ankle dislocation (which tends to carry a high
risk of neurovascular compromise).
Since this patient does not have an open fracture,
dislocation or evidence of neurovascular compromise,
his stable fracture does not require an immediate
orthopedic intervention. Therefore, this patient may be
immobilized in an appropriate splint and sent home with
an orthopedic referral for definitive casting. A posterior
ankle splint would probably not be adequate
immobilization by itself for an ankle fracture.
Review splint types.
What does this mortise view reveal that may not
have be very evident on the 2 previous views?
Radiographic interpretation: There is a moderate
amount of soft tissue swelling over the lateral malleolus.
The AP and lateral views do not reveal any obvious
fractures. However, there is a subtle widening of the
medial aspect of the distal fibular growth plate (physis)
on the mortise view. Comparative views and/or stress
views would confirm that this is a fracture versus a
normal growth plate closure.
Questions:
a) Does this patient require immediate orthopedic
intervention or can he be sent home from the
Emergency Department with an out-patient orthopedic
referral?
b) If you would send this patient home, what type of
dressing or splint would you apply?
Discussion & Teaching Points:
This patient has sustained a nondisplaced
Salter-Harris type I fracture of the distal fibula (lateral
malleolus). Clinical and or radiographic criteria that
would warrant immediate orthopedic intervention
include:
a) An open fracture.
b) Any type of injury with neurovascular
compromise.
c) Any unstable fracture (which would be difficult to
adequately immobilize in a splint).
d) Any ankle dislocation (which tends to carry a high
risk of neurovascular compromise).
Since this patient does not have an open fracture,
dislocation or evidence of neurovascular compromise,
his stable fracture does not require an immediate
orthopedic intervention. Therefore, this patient may be
immobilized in an appropriate splint and sent home with
an orthopedic referral for definitive casting. A posterior
ankle splint would probably not be adequate
immobilization by itself for an ankle fracture.
Review splint types.
 The posterior splint is on the left. The sugartong (or
stirrup) splint is on the right. An ankle stirrup splint
would provide better immobilization, since it protects
against inversion-eversion and to some degree also
protects against a fair degree of flexion-extension.
The stirrup splint can also be combined with the
posterior splint to provide maximal immobilization and
protection against further trauma to the injured ankle.
Patients should be told to refrain from weight-bearing
(use crutches) and to elevate the injured extremity as
much as possible.
References:
Anderson AC. Injury: Ankle (Chapter 35). In:
Fleisher GR & Ludwig S (eds). Textbook of Pediatric
Emergency Medicine, Third Edition. Baltimore,
Williams & Wilkins, 1993, pp. 259-267.
Harris JH, Harris WH, Novelline RA. The Ankle
(Chapter 14). In: The Radiology of Emergency
Medicine. Williams & Wilkins, 1993, pp. 966-1009.
Jackson JL, Linakis JG. Ankle and Foot Injuries. In:
Barkin RM, et al (eds). Pediatric Emergency Medicine:
Concepts and Clinical Practice. St. Louis, Mosby Year
Book, 1993, pp. 366-375.
Pigman EC, Klug RK, Sanford S, et al. Evaluation
of the Ottawa clinical decision rules for the use of
radiography in acute ankle and midfoot injuries in the
emergency department: An independent site
assessment. Ann Emerg Med 1994;24;41-45.
Reisdorff EJ, Cowling KM. The injured ankle: New
twists to a familiar problem. Emerg Med Reports
1995;16;39-48.
Simon RR, Koenigs SJ. The Ankle (Chapter 30).
In: Emergency Orthopedics, The Extremities, Third
Edition. Norwalk, Appleton & Lange, 1995, pp.
477-489.
Stiell IG, McDowell I, Nair RC, et al. Use of
radiography in acute ankle injuries: Physician's
attitudes and practice. Can Med Assoc J
1992;147:1671-1678.
Stiell IG, McKnight RD, Greenberg GH. Decision
rules for use of radiography in acute ankle injuries:
Refinement and prospective evaluation. JAMA
1993;269:1127-1132.
Swischuk LE. The Extremities (Chapter 4). In:
Emergency Imaging of the Acutely Ill or Injured Child,
Third Edition. Baltimore, Wiliiams & Wilkins, 1994, pp.
528-548.
The posterior splint is on the left. The sugartong (or
stirrup) splint is on the right. An ankle stirrup splint
would provide better immobilization, since it protects
against inversion-eversion and to some degree also
protects against a fair degree of flexion-extension.
The stirrup splint can also be combined with the
posterior splint to provide maximal immobilization and
protection against further trauma to the injured ankle.
Patients should be told to refrain from weight-bearing
(use crutches) and to elevate the injured extremity as
much as possible.
References:
Anderson AC. Injury: Ankle (Chapter 35). In:
Fleisher GR & Ludwig S (eds). Textbook of Pediatric
Emergency Medicine, Third Edition. Baltimore,
Williams & Wilkins, 1993, pp. 259-267.
Harris JH, Harris WH, Novelline RA. The Ankle
(Chapter 14). In: The Radiology of Emergency
Medicine. Williams & Wilkins, 1993, pp. 966-1009.
Jackson JL, Linakis JG. Ankle and Foot Injuries. In:
Barkin RM, et al (eds). Pediatric Emergency Medicine:
Concepts and Clinical Practice. St. Louis, Mosby Year
Book, 1993, pp. 366-375.
Pigman EC, Klug RK, Sanford S, et al. Evaluation
of the Ottawa clinical decision rules for the use of
radiography in acute ankle and midfoot injuries in the
emergency department: An independent site
assessment. Ann Emerg Med 1994;24;41-45.
Reisdorff EJ, Cowling KM. The injured ankle: New
twists to a familiar problem. Emerg Med Reports
1995;16;39-48.
Simon RR, Koenigs SJ. The Ankle (Chapter 30).
In: Emergency Orthopedics, The Extremities, Third
Edition. Norwalk, Appleton & Lange, 1995, pp.
477-489.
Stiell IG, McDowell I, Nair RC, et al. Use of
radiography in acute ankle injuries: Physician's
attitudes and practice. Can Med Assoc J
1992;147:1671-1678.
Stiell IG, McKnight RD, Greenberg GH. Decision
rules for use of radiography in acute ankle injuries:
Refinement and prospective evaluation. JAMA
1993;269:1127-1132.
Swischuk LE. The Extremities (Chapter 4). In:
Emergency Imaging of the Acutely Ill or Injured Child,
Third Edition. Baltimore, Wiliiams & Wilkins, 1994, pp.
528-548.
Return to Radiology Cases In Ped Emerg Med Case Selection Page
Return to Univ. Hawaii Dept. Pediatrics Home Page
 The black arrow points to the region of maximum
tenderness. There is no tenderness along the inferior
tip of the lateral malleolus or over the bony prominence
of the lateral malleolus. There is no tenderness along
the medial aspect of the ankle or along the proximal
aspects of both the tibial and fibular shafts. The
squeeze test over the distal tibia-fibula region does not
produce any pain. Both the anterior drawer and talar tilt
maneuvers are within normal limits when compared to
the nonaffected ankle.
Questions:
a) Has this patient sustained a typical ankle sprain?
b) What is the typical mechanism of injury for the
majority of ankle sprains sustained during sporting
events?
c) Which ankle ligament is most commonly sprained
during an inversion injury, and where on the ankle
should one palpate to check for tenderness to this
ligament?
d) Describe the anterior drawer test and what
specifically does this maneuver test for?
e) Describe the talar tilt test and what specifically
does this maneuver test for?
f) What is the syndesmosis, and how does one
examine for possible syndesmotic injuries?
Discussion & Teaching Points:
Ankle injuries are one of the most common
sports-related orthopedic injuries seen in the
Emergency Department. These types of injuries are
most commonly sustained in patients between 15 - 35
years of age. The majority of ankle sprains (up to 85%)
are due to inversion injuries while only 15% are due to
eversion-related injuries. There are 3 lateral ankle
ligaments and one broad, fan-shaped medial ligament.
Review the ligaments.
The black arrow points to the region of maximum
tenderness. There is no tenderness along the inferior
tip of the lateral malleolus or over the bony prominence
of the lateral malleolus. There is no tenderness along
the medial aspect of the ankle or along the proximal
aspects of both the tibial and fibular shafts. The
squeeze test over the distal tibia-fibula region does not
produce any pain. Both the anterior drawer and talar tilt
maneuvers are within normal limits when compared to
the nonaffected ankle.
Questions:
a) Has this patient sustained a typical ankle sprain?
b) What is the typical mechanism of injury for the
majority of ankle sprains sustained during sporting
events?
c) Which ankle ligament is most commonly sprained
during an inversion injury, and where on the ankle
should one palpate to check for tenderness to this
ligament?
d) Describe the anterior drawer test and what
specifically does this maneuver test for?
e) Describe the talar tilt test and what specifically
does this maneuver test for?
f) What is the syndesmosis, and how does one
examine for possible syndesmotic injuries?
Discussion & Teaching Points:
Ankle injuries are one of the most common
sports-related orthopedic injuries seen in the
Emergency Department. These types of injuries are
most commonly sustained in patients between 15 - 35
years of age. The majority of ankle sprains (up to 85%)
are due to inversion injuries while only 15% are due to
eversion-related injuries. There are 3 lateral ankle
ligaments and one broad, fan-shaped medial ligament.
Review the ligaments.
 Although ankle sprains are common in older
adolescent patients and young adults, isolated ankle
sprains are not very common in younger children and
in preadolescent patients. The physis (growth plate) in
these younger children is much weaker than the
surrounding ligaments, and is thus more susceptible to
injury. Therefore in the pediatric population, injuries
involving the growth plates (Salter-Harris injuries) must
also be considered in addition to ligament sprains.
The anterior talofibular ligament (ATFL) is the
weakest of the 3 lateral ligaments and is the most
commonly injured of the lateral ankle ligaments. (Note
that ATFL can also stand for anterior tibiofibular
ligament, however, in this case, ATFL will be used to
stand for anterior talofibular ligament.) 65% of lateral
ligament sprains are confined to the ATFL alone, while
20% have concomitant calcaneofibular ligament (CFL)
tears. The ATFL can be palpated just inferior and
anterior to the distal most aspect of the lateral
malleolus.
Review ATFL location.
Although ankle sprains are common in older
adolescent patients and young adults, isolated ankle
sprains are not very common in younger children and
in preadolescent patients. The physis (growth plate) in
these younger children is much weaker than the
surrounding ligaments, and is thus more susceptible to
injury. Therefore in the pediatric population, injuries
involving the growth plates (Salter-Harris injuries) must
also be considered in addition to ligament sprains.
The anterior talofibular ligament (ATFL) is the
weakest of the 3 lateral ligaments and is the most
commonly injured of the lateral ankle ligaments. (Note
that ATFL can also stand for anterior tibiofibular
ligament, however, in this case, ATFL will be used to
stand for anterior talofibular ligament.) 65% of lateral
ligament sprains are confined to the ATFL alone, while
20% have concomitant calcaneofibular ligament (CFL)
tears. The ATFL can be palpated just inferior and
anterior to the distal most aspect of the lateral
malleolus.
Review ATFL location.
 The white arrow points to the region of the ATFL.
Because the patient in this case has point tenderness in
an area other than over the ATFL, he has therefore not
sustained a typical ankle sprain. In comparison to
these lateral ligaments, the medial, deltoid ligament has
a fair degree of elasticity and is much more resistant to
tears.
Most injuries also occur while the ankle joint is in
plantar flexion rather than in dorsiflexion. Anatomically,
the talar dome is wedge-shaped, with the anterior
aspect of the talus being wider than the posterior
aspect. During dorsiflexion, this wider, anterior aspect
of the talus is engaged within the mortise (formed by
the distal tibia and fibula), and the joint is very stable.
However during plantar flexion, the narrower, posterior
aspect of the talus becomes engaged in the ankle
mortise.
Review joint space diagram.
The white arrow points to the region of the ATFL.
Because the patient in this case has point tenderness in
an area other than over the ATFL, he has therefore not
sustained a typical ankle sprain. In comparison to
these lateral ligaments, the medial, deltoid ligament has
a fair degree of elasticity and is much more resistant to
tears.
Most injuries also occur while the ankle joint is in
plantar flexion rather than in dorsiflexion. Anatomically,
the talar dome is wedge-shaped, with the anterior
aspect of the talus being wider than the posterior
aspect. During dorsiflexion, this wider, anterior aspect
of the talus is engaged within the mortise (formed by
the distal tibia and fibula), and the joint is very stable.
However during plantar flexion, the narrower, posterior
aspect of the talus becomes engaged in the ankle
mortise.
Review joint space diagram.
 Note the obvious widening of the joint space during
plantar flexion on the left compared to dorsiflexion on
the right. Thus, with this understanding of the
articulation of the talus within the mortise, it is not
surprising that most ankle injuries occur while the ankle
is in plantar flexion, rather than in dorsiflexion.
The last part of the clinical examination of an injured
ankle involves assessing the stability of the ankle joint.
The two maneuvers that can be performed to assess
the stability of the ankle joint are the anterior drawer
and talar tilt maneuvers. Keep in mind that the ability to
perform these tests and the results immediately after an
injury may be limited by swelling, pain and muscle
spasm. Do not attempt to perform either of these tests
if there is an obvious deformity of the ankle suggestive
of a possible ankle fracture.
The ATFL ligament normally prevents the anterior
subluxation of the talus from the mortise. The talus
may be subluxed anteriorly whenever the ATFL is
partially ruptured (second-degree sprain) or completely
ruptured (third-degree sprain). The anterior drawer
maneuver assesses the integrity of the ATFL. Since
the ATFL is usually the first ligament to be injured in a
typical inversion injury, some physicians feel that if this
anterior drawer test is negative, it is then unnecessary
to perform the talar tilt maneuver (since the talar tilt
stress test is positive only if both the ATFL and the CFL
are injured). To perform the anterior drawer maneuver,
the patient can either be supine or sitting down, with the
ankle in neutral position. One hand of the examiner
cups the heel of the affected ankle (and attempts to pull
the foot anteriorly), while the other hand braces along
the anterior aspect of the lower leg.
Review drawer sign maneuver.
Note the obvious widening of the joint space during
plantar flexion on the left compared to dorsiflexion on
the right. Thus, with this understanding of the
articulation of the talus within the mortise, it is not
surprising that most ankle injuries occur while the ankle
is in plantar flexion, rather than in dorsiflexion.
The last part of the clinical examination of an injured
ankle involves assessing the stability of the ankle joint.
The two maneuvers that can be performed to assess
the stability of the ankle joint are the anterior drawer
and talar tilt maneuvers. Keep in mind that the ability to
perform these tests and the results immediately after an
injury may be limited by swelling, pain and muscle
spasm. Do not attempt to perform either of these tests
if there is an obvious deformity of the ankle suggestive
of a possible ankle fracture.
The ATFL ligament normally prevents the anterior
subluxation of the talus from the mortise. The talus
may be subluxed anteriorly whenever the ATFL is
partially ruptured (second-degree sprain) or completely
ruptured (third-degree sprain). The anterior drawer
maneuver assesses the integrity of the ATFL. Since
the ATFL is usually the first ligament to be injured in a
typical inversion injury, some physicians feel that if this
anterior drawer test is negative, it is then unnecessary
to perform the talar tilt maneuver (since the talar tilt
stress test is positive only if both the ATFL and the CFL
are injured). To perform the anterior drawer maneuver,
the patient can either be supine or sitting down, with the
ankle in neutral position. One hand of the examiner
cups the heel of the affected ankle (and attempts to pull
the foot anteriorly), while the other hand braces along
the anterior aspect of the lower leg.
Review drawer sign maneuver.
 If the foot of the affected ankle can be pulled forward
by more than 3 - 5 mm (or if the affected ankle can be
subluxed more forward than the nonaffected side),
suspect a rupture of the ATFL.
The talar tilt test assesses the integrity of the CFL.
To perform this maneuver the patient can again be
either sitting down or supine, with the ankle in neutral
position. While one hand of the examiner holds the
lower leg stationary, the other hand gently attempts to
invert the ankle.
Review talar tilt maneuver.
If the foot of the affected ankle can be pulled forward
by more than 3 - 5 mm (or if the affected ankle can be
subluxed more forward than the nonaffected side),
suspect a rupture of the ATFL.
The talar tilt test assesses the integrity of the CFL.
To perform this maneuver the patient can again be
either sitting down or supine, with the ankle in neutral
position. While one hand of the examiner holds the
lower leg stationary, the other hand gently attempts to
invert the ankle.
Review talar tilt maneuver.
 Greater than 10 degrees of difference in the talar tilt
when compared to the nonaffected side is suggestive of
an injury to the CFL.
Proximal to the lateral and medial ankle ligaments,
the distal tibia and distal fibula are connected to each
other by a series of tough fibrous structures collectively
referred to as the tibiofibular syndesmosis. The three
individual components which make-up this syndesmosis
include: a) anterior tibiofibular ligament, b) posterior
tibiofibular ligament, and c) intraosseous membrane.
Review syndesmosis anatomy.
Greater than 10 degrees of difference in the talar tilt
when compared to the nonaffected side is suggestive of
an injury to the CFL.
Proximal to the lateral and medial ankle ligaments,
the distal tibia and distal fibula are connected to each
other by a series of tough fibrous structures collectively
referred to as the tibiofibular syndesmosis. The three
individual components which make-up this syndesmosis
include: a) anterior tibiofibular ligament, b) posterior
tibiofibular ligament, and c) intraosseous membrane.
Review syndesmosis anatomy.
 Note that on this diagram, the PTFL stands for the
posterior talofibular ligament (not the posterior
tibiofibular ligament). The posterior tibiofibular ligament
is NOT drawn on this diagramatic view.
Clinically one can check for injuries of the tibiofibular
syndesmosis by the squeeze test. To perform this test,
the examiner firmly grasps the patient's lower leg
(around the lower aspect of the calf), and gently
squeezes the tibia and fibula together.
Review squeeze test.
Note that on this diagram, the PTFL stands for the
posterior talofibular ligament (not the posterior
tibiofibular ligament). The posterior tibiofibular ligament
is NOT drawn on this diagramatic view.
Clinically one can check for injuries of the tibiofibular
syndesmosis by the squeeze test. To perform this test,
the examiner firmly grasps the patient's lower leg
(around the lower aspect of the calf), and gently
squeezes the tibia and fibula together.
Review squeeze test.
 Provided that there are no fractures of the tibial or
fibular shafts, if ankle pain can be elicited by this
squeeze maneuver, one should suspect an injury to one
or more of the components of the tibiofibular
syndesmosis.
Questions:
a) What are some clinical criteria that would warrant
a radiographic examination of an injured ankle?
b) What are the 3 standard radiographic views that
are obtained on patients with ankle injuries?
c) When do the distal tibial and distal fibular
epiphyses appear, and by what age do these epiphyses
fuse to the adjacent metaphyses?
Discussion & Teaching Points
It is estimated that over $500 million dollars are
spent each year on ankle radiographs. However the
majority (up to 85%) of these radiographs are negative.
In 1992, a Canadian study suggested the adaptation of
the Ottawa ankle rules, which could be used to order
ankle radiographs based on selected clinical criteria. It
is important to remember that this study excluded
patients younger than 18 years of age. Therefore,
since the Ottawa study did not include growth plate
injuries, one should not strictly adhere to these rules
when deciding whether or not to obtain a radiograph on
a pediatric patient. Based on these Ottawa ankle rules,
clinical indications that would warrant a radiographic
evaluation would include any one of the following
criteria:
a) Inability to bear weight both immediately after the
injury and in the Emergency Department.
b) Bony tenderness over the posterior edge, tip or
distal 6 cm of the lateral malleolus.
c) Bony tenderness over the posterior edge, tip or
distal 6 cm of the medial malleolus.
d) Tenderness over the base of the 5th metatarsal.
A complete, standard radiograph examination of the
ankle should include 3 views (AP, lateral, and a mortise
view).
Review ankle views.
Provided that there are no fractures of the tibial or
fibular shafts, if ankle pain can be elicited by this
squeeze maneuver, one should suspect an injury to one
or more of the components of the tibiofibular
syndesmosis.
Questions:
a) What are some clinical criteria that would warrant
a radiographic examination of an injured ankle?
b) What are the 3 standard radiographic views that
are obtained on patients with ankle injuries?
c) When do the distal tibial and distal fibular
epiphyses appear, and by what age do these epiphyses
fuse to the adjacent metaphyses?
Discussion & Teaching Points
It is estimated that over $500 million dollars are
spent each year on ankle radiographs. However the
majority (up to 85%) of these radiographs are negative.
In 1992, a Canadian study suggested the adaptation of
the Ottawa ankle rules, which could be used to order
ankle radiographs based on selected clinical criteria. It
is important to remember that this study excluded
patients younger than 18 years of age. Therefore,
since the Ottawa study did not include growth plate
injuries, one should not strictly adhere to these rules
when deciding whether or not to obtain a radiograph on
a pediatric patient. Based on these Ottawa ankle rules,
clinical indications that would warrant a radiographic
evaluation would include any one of the following
criteria:
a) Inability to bear weight both immediately after the
injury and in the Emergency Department.
b) Bony tenderness over the posterior edge, tip or
distal 6 cm of the lateral malleolus.
c) Bony tenderness over the posterior edge, tip or
distal 6 cm of the medial malleolus.
d) Tenderness over the base of the 5th metatarsal.
A complete, standard radiograph examination of the
ankle should include 3 views (AP, lateral, and a mortise
view).
Review ankle views.
 a) AP view: There are several findings that can be
observed on the AP view. The tip of the lateral
malleolus normally extends more distally than the tip of
the medial malleolus. The syndesmosis of the ankle
joint normally causes an overlap of the medial aspect of
the distal fibula and the lateral aspect of the distal tibia
on this AP view. Therefore, subtle fractures involving
either the lateral aspect of the distal tibia or the medial
aspect of the distal fibula (i.e., between the tibia and
fibula) may be difficult to visualize on this AP view alone
because of the overlap. It is a common pitfall to miss a
Salter Harris Type III fracture of the distal lateral tibia
because it is obscured by the overlapping fibula.
b) Lateral view: On a true lateral view, the malleoli
should be superimposed upon one another. The lateral
view provides a better view of the posterior aspect of
the distal tibia and fibula, the talus, calcaneus and the
base of the 5th metatarsal.
c) Mortise view: To obtain a better view of the
ankle mortise, the patient's leg must be internally
rotated just enough so that the lateral malleolus (which
is normally posterior to the medial malleolus), is on the
same horizontal plane as the medial malleolus, and a
line drawn through both malleoli would be parallel to the
tabletop. Usually this only requires approximately 10 -
20 degrees of internal rotation. In other words, whe
n viewing the mortise view, the tibia and fibula must be
viewed without superimposition on each other. This
mortise view represents a true AP projection of the
ankle mortise and also provides a good visualization of
the talar dome (to rule-out osteochondral talar dome
fractures). The clear joint space [formed by the
talofibular joint, the superior space between the dome
of the talus & the tibial plafond (the inferior articulating
surface of the tibia) and the tibiotalar joint] should all
uniformly measure 3 - 4 mm. A difference of greater
than 2 mm (i.e., the joint space width varies by more
than 2 mm. Eg., Joint space measures 2 mm at lateral
part of joint and 5 mm at medial side of joint.) is
suggestive of mortise instability.
If all of the above 3 views appear normal in a patient
with a high clinical suspicion of a fracture, one should
then obtain internal and external oblique views of the
ankle to obtain additional views of the distal tibia and
distal fibula. To obtain such views, the patient's leg is
rotated 45 degrees internally, then 45 degree externally.
The epiphyses of the distal tibia and fibula both
appear by 2 years of age. The physis of the distal tibia
fuses to its adjacent metaphysis by 18 years of age.
The physis of the distal fibula fuses to its adjacent
metaphysis by 20 years of age. Therefore, growth plate
injuries should still be considered as a possibility in any
patient up to 20 years of age. If one is unsure if a
radiolucent line involving the distal tibia or fibula
represents either a physis or an actual fracture,
consider obtaining a comparison view of the
nonaffected ankle.
An x-ray of the patient's ankle was obtained.
Review our patient's ankle radiographs.
a) AP view: There are several findings that can be
observed on the AP view. The tip of the lateral
malleolus normally extends more distally than the tip of
the medial malleolus. The syndesmosis of the ankle
joint normally causes an overlap of the medial aspect of
the distal fibula and the lateral aspect of the distal tibia
on this AP view. Therefore, subtle fractures involving
either the lateral aspect of the distal tibia or the medial
aspect of the distal fibula (i.e., between the tibia and
fibula) may be difficult to visualize on this AP view alone
because of the overlap. It is a common pitfall to miss a
Salter Harris Type III fracture of the distal lateral tibia
because it is obscured by the overlapping fibula.
b) Lateral view: On a true lateral view, the malleoli
should be superimposed upon one another. The lateral
view provides a better view of the posterior aspect of
the distal tibia and fibula, the talus, calcaneus and the
base of the 5th metatarsal.
c) Mortise view: To obtain a better view of the
ankle mortise, the patient's leg must be internally
rotated just enough so that the lateral malleolus (which
is normally posterior to the medial malleolus), is on the
same horizontal plane as the medial malleolus, and a
line drawn through both malleoli would be parallel to the
tabletop. Usually this only requires approximately 10 -
20 degrees of internal rotation. In other words, whe
n viewing the mortise view, the tibia and fibula must be
viewed without superimposition on each other. This
mortise view represents a true AP projection of the
ankle mortise and also provides a good visualization of
the talar dome (to rule-out osteochondral talar dome
fractures). The clear joint space [formed by the
talofibular joint, the superior space between the dome
of the talus & the tibial plafond (the inferior articulating
surface of the tibia) and the tibiotalar joint] should all
uniformly measure 3 - 4 mm. A difference of greater
than 2 mm (i.e., the joint space width varies by more
than 2 mm. Eg., Joint space measures 2 mm at lateral
part of joint and 5 mm at medial side of joint.) is
suggestive of mortise instability.
If all of the above 3 views appear normal in a patient
with a high clinical suspicion of a fracture, one should
then obtain internal and external oblique views of the
ankle to obtain additional views of the distal tibia and
distal fibula. To obtain such views, the patient's leg is
rotated 45 degrees internally, then 45 degree externally.
The epiphyses of the distal tibia and fibula both
appear by 2 years of age. The physis of the distal tibia
fuses to its adjacent metaphysis by 18 years of age.
The physis of the distal fibula fuses to its adjacent
metaphysis by 20 years of age. Therefore, growth plate
injuries should still be considered as a possibility in any
patient up to 20 years of age. If one is unsure if a
radiolucent line involving the distal tibia or fibula
represents either a physis or an actual fracture,
consider obtaining a comparison view of the
nonaffected ankle.
An x-ray of the patient's ankle was obtained.
Review our patient's ankle radiographs.
 How would you interpret these 2 views? Oblique
and mortise views were also obtained because of the
physical exam findings.
Review mortise view.
How would you interpret these 2 views? Oblique
and mortise views were also obtained because of the
physical exam findings.
Review mortise view.
 What does this mortise view reveal that may not
have be very evident on the 2 previous views?
Radiographic interpretation: There is a moderate
amount of soft tissue swelling over the lateral malleolus.
The AP and lateral views do not reveal any obvious
fractures. However, there is a subtle widening of the
medial aspect of the distal fibular growth plate (physis)
on the mortise view. Comparative views and/or stress
views would confirm that this is a fracture versus a
normal growth plate closure.
Questions:
a) Does this patient require immediate orthopedic
intervention or can he be sent home from the
Emergency Department with an out-patient orthopedic
referral?
b) If you would send this patient home, what type of
dressing or splint would you apply?
Discussion & Teaching Points:
This patient has sustained a nondisplaced
Salter-Harris type I fracture of the distal fibula (lateral
malleolus). Clinical and or radiographic criteria that
would warrant immediate orthopedic intervention
include:
a) An open fracture.
b) Any type of injury with neurovascular
compromise.
c) Any unstable fracture (which would be difficult to
adequately immobilize in a splint).
d) Any ankle dislocation (which tends to carry a high
risk of neurovascular compromise).
Since this patient does not have an open fracture,
dislocation or evidence of neurovascular compromise,
his stable fracture does not require an immediate
orthopedic intervention. Therefore, this patient may be
immobilized in an appropriate splint and sent home with
an orthopedic referral for definitive casting. A posterior
ankle splint would probably not be adequate
immobilization by itself for an ankle fracture.
Review splint types.
What does this mortise view reveal that may not
have be very evident on the 2 previous views?
Radiographic interpretation: There is a moderate
amount of soft tissue swelling over the lateral malleolus.
The AP and lateral views do not reveal any obvious
fractures. However, there is a subtle widening of the
medial aspect of the distal fibular growth plate (physis)
on the mortise view. Comparative views and/or stress
views would confirm that this is a fracture versus a
normal growth plate closure.
Questions:
a) Does this patient require immediate orthopedic
intervention or can he be sent home from the
Emergency Department with an out-patient orthopedic
referral?
b) If you would send this patient home, what type of
dressing or splint would you apply?
Discussion & Teaching Points:
This patient has sustained a nondisplaced
Salter-Harris type I fracture of the distal fibula (lateral
malleolus). Clinical and or radiographic criteria that
would warrant immediate orthopedic intervention
include:
a) An open fracture.
b) Any type of injury with neurovascular
compromise.
c) Any unstable fracture (which would be difficult to
adequately immobilize in a splint).
d) Any ankle dislocation (which tends to carry a high
risk of neurovascular compromise).
Since this patient does not have an open fracture,
dislocation or evidence of neurovascular compromise,
his stable fracture does not require an immediate
orthopedic intervention. Therefore, this patient may be
immobilized in an appropriate splint and sent home with
an orthopedic referral for definitive casting. A posterior
ankle splint would probably not be adequate
immobilization by itself for an ankle fracture.
Review splint types.
 The posterior splint is on the left. The sugartong (or
stirrup) splint is on the right. An ankle stirrup splint
would provide better immobilization, since it protects
against inversion-eversion and to some degree also
protects against a fair degree of flexion-extension.
The stirrup splint can also be combined with the
posterior splint to provide maximal immobilization and
protection against further trauma to the injured ankle.
Patients should be told to refrain from weight-bearing
(use crutches) and to elevate the injured extremity as
much as possible.
References:
Anderson AC. Injury: Ankle (Chapter 35). In:
Fleisher GR & Ludwig S (eds). Textbook of Pediatric
Emergency Medicine, Third Edition. Baltimore,
Williams & Wilkins, 1993, pp. 259-267.
Harris JH, Harris WH, Novelline RA. The Ankle
(Chapter 14). In: The Radiology of Emergency
Medicine. Williams & Wilkins, 1993, pp. 966-1009.
Jackson JL, Linakis JG. Ankle and Foot Injuries. In:
Barkin RM, et al (eds). Pediatric Emergency Medicine:
Concepts and Clinical Practice. St. Louis, Mosby Year
Book, 1993, pp. 366-375.
Pigman EC, Klug RK, Sanford S, et al. Evaluation
of the Ottawa clinical decision rules for the use of
radiography in acute ankle and midfoot injuries in the
emergency department: An independent site
assessment. Ann Emerg Med 1994;24;41-45.
Reisdorff EJ, Cowling KM. The injured ankle: New
twists to a familiar problem. Emerg Med Reports
1995;16;39-48.
Simon RR, Koenigs SJ. The Ankle (Chapter 30).
In: Emergency Orthopedics, The Extremities, Third
Edition. Norwalk, Appleton & Lange, 1995, pp.
477-489.
Stiell IG, McDowell I, Nair RC, et al. Use of
radiography in acute ankle injuries: Physician's
attitudes and practice. Can Med Assoc J
1992;147:1671-1678.
Stiell IG, McKnight RD, Greenberg GH. Decision
rules for use of radiography in acute ankle injuries:
Refinement and prospective evaluation. JAMA
1993;269:1127-1132.
Swischuk LE. The Extremities (Chapter 4). In:
Emergency Imaging of the Acutely Ill or Injured Child,
Third Edition. Baltimore, Wiliiams & Wilkins, 1994, pp.
528-548.
The posterior splint is on the left. The sugartong (or
stirrup) splint is on the right. An ankle stirrup splint
would provide better immobilization, since it protects
against inversion-eversion and to some degree also
protects against a fair degree of flexion-extension.
The stirrup splint can also be combined with the
posterior splint to provide maximal immobilization and
protection against further trauma to the injured ankle.
Patients should be told to refrain from weight-bearing
(use crutches) and to elevate the injured extremity as
much as possible.
References:
Anderson AC. Injury: Ankle (Chapter 35). In:
Fleisher GR & Ludwig S (eds). Textbook of Pediatric
Emergency Medicine, Third Edition. Baltimore,
Williams & Wilkins, 1993, pp. 259-267.
Harris JH, Harris WH, Novelline RA. The Ankle
(Chapter 14). In: The Radiology of Emergency
Medicine. Williams & Wilkins, 1993, pp. 966-1009.
Jackson JL, Linakis JG. Ankle and Foot Injuries. In:
Barkin RM, et al (eds). Pediatric Emergency Medicine:
Concepts and Clinical Practice. St. Louis, Mosby Year
Book, 1993, pp. 366-375.
Pigman EC, Klug RK, Sanford S, et al. Evaluation
of the Ottawa clinical decision rules for the use of
radiography in acute ankle and midfoot injuries in the
emergency department: An independent site
assessment. Ann Emerg Med 1994;24;41-45.
Reisdorff EJ, Cowling KM. The injured ankle: New
twists to a familiar problem. Emerg Med Reports
1995;16;39-48.
Simon RR, Koenigs SJ. The Ankle (Chapter 30).
In: Emergency Orthopedics, The Extremities, Third
Edition. Norwalk, Appleton & Lange, 1995, pp.
477-489.
Stiell IG, McDowell I, Nair RC, et al. Use of
radiography in acute ankle injuries: Physician's
attitudes and practice. Can Med Assoc J
1992;147:1671-1678.
Stiell IG, McKnight RD, Greenberg GH. Decision
rules for use of radiography in acute ankle injuries:
Refinement and prospective evaluation. JAMA
1993;269:1127-1132.
Swischuk LE. The Extremities (Chapter 4). In:
Emergency Imaging of the Acutely Ill or Injured Child,
Third Edition. Baltimore, Wiliiams & Wilkins, 1994, pp.
528-548.