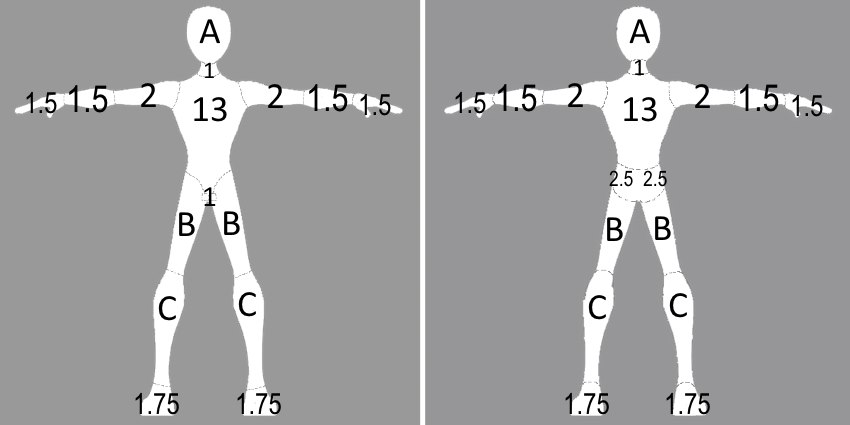
Figure 1. Modified Lund and Browder chart for infants and children using the table values below

A 3 year old male is brought to the emergency department after suffering burns to the right arm when a hot cup of coffee spilled on him. His family applied gel from an Aloe plant to the burn before coming to the ED. He is otherwise healthy and his immunizations are up to date.
Exam: VS T 37.5, P120, R20, BP (unobtainable, crying), oxygen saturation 100% in room air. Weight 15 kg. He is alert and active, in moderate distress. His right forearm appears mostly red. It is painful and blanches upon palpation. One smaller intact blister and one large ruptured blister are present on the dorsal aspect of the right forearm. The blistered surface area is estimated to be 2% and the non-blistered red area is estimated to be 2% for a total body surface area (TBSA) of 4%.
The physician recommends an intranal dose of fentanyl, which is administered. Cool, sterile, saline-soaked gauze is applied to the wound surface and the open areas are gently cleansed with saline. Tissue from the ruptured blister is removed and the intact blister is flimsy so it is drained and removed. Antibiotic ointment is applied to areas of partial thickness burns and the burns are dressed. He is discharged with instructions for the parents to gently cleanse the burns with mild soap and water, reapply the antibiotic ointment, and change the dressing each day. His burn healed completely without complications in five weeks.
Fire or burn injuries are the fourth leading cause of accidental death in US children. In 2011, according to the CDC (Centers for Disease Control and Prevention), almost 130,000 children sought medical treatment for burns in the US. Children from birth to age 4 account for nearly 50% of all pediatric burns (1). After age 4, the incidence of burn injuries declines only to rise again in adolescence as individuals enter the work force (2).
Skin is the largest organ in the body. It consists of two main layers: the epidermis and the dermis. The epidermis is the outermost layer of the skin. It is composed of keratinocytes that mature and differentiate as they reach the skin surface. The superficial layer of anuclear keratinocytes is called the stratum corneum. The stratum corneum acts as a barrier that prevents the loss of water and electrolytes as well as the entrance of microorganisms. Other cells found in the epidermis are melanocytes (which gives the skin its color), Merkel cells (which are pressure receptors), and Langerhans cells (which participate in the skin's immune response).
Deep to the epidermis is the dermis. The dermis is made up of dense fibroelastic connective tissue containing collagen and elastic fibers, and ground substance, an extracellular gel. The dermis contains an extensive neurovascular network and skin appendages (glands and hair follicles) that communicate with the overlying epidermis. Beneath the dermis is subcutaneous tissue consisting of adipose tissue.
Burns are classified according to the depth of injury. First degree burns are limited to the epidermis. A sunburn is an example of a first degree burn. These burns are red, dry, and painful with no epidermal sloughing or blistering. Blanching is visible when pressure is applied to the wound. First degree burns do not lead to scarring and require only local wound care. Second degree (partial thickness) burns extend into the dermis with some residual dermis remaining viable. These burns are pink to pale pink, moist, and painful. They blanch on application of pressure. Epidermal sloughing and blisters are present. In third degree (full thickness) burns, the entire dermis is destroyed leaving subcutaneous tissue exposed. These burns appear white, mottled, or charred. They are dry and may be firm or leathery. Third degree burns do not blanch and are not painful. Fourth degree (transmural) burns extend through the subcutaneous tissue, exposing muscle and bone. They are often associated with a lethal injury.
Most pediatric burn injuries occur at home and are largely preventable. In children younger than 4 years old, the most frequent burns are scalds. These injuries are the result of exposure to hot liquids (pulling pots off the stove, spilling hot beverages, or hot tap water). The second most frequent cause of burn injuries is contact with hot objects (the stovetop, a hot oven door, clothes irons, or curling irons). Furthermore, infants, toddlers, and small children may not be able to escape the burning object as well as an older child. Prolonged duration of contact may increase the severity of the injury. In older children, the majority of burns are due to fires and environmental causes such as hot barbecue grills, hot mufflers, or engines.
Although the majority of pediatric burns are accidental, approximately 20% of burn injuries occur as a result of child abuse (3). If a non-accidental burn is suspected, the family should be questioned carefully. Any inconsistencies in the history of the injury suggest the possibility of child abuse and should be reported to the child protective authorities as required by law (4). Chronically abused children may have a depressed affect. Furthermore, the pattern of the burn may be suspicious of intentional injury. Scalding burns of the extremities in which the entire foot or hand is burned, with a glove or stocking pattern and lack of splash marks, suggest forced immersion into hot water. Additionally, burns on the back, buttock, or both soles of the feet are highly suspicious for child abuse. The depth of the burn is another factor to keep in mind when abuse is being considered. Partial thickness burns commonly result from accidental scalding. Full thickness burns caused by scalding suggest sustained contact with hot water. Small area, full thickness burns suggest injury from a cigarette. Evidence of other trauma, such as bruising or numerous healed wounds, should be documented.
The first step in management of a burn injury is assessment of life-threatening conditions. The airway must be evaluated immediately for compromise in the case of burns caused by flame or history of smoke exposure. Smoke inhalation can result in severe inflammation of the airways and lungs. Classic signs associated with significant smoke inhalation are burns to the face or nasal hairs and/or carbonaceous sputum (4). Because the airway can swell rapidly, this condition must be treated aggressively and quickly to prevent airway obstruction. Immediate tracheal intubation is indicated if the patient shows signs of laryngeal edema such as hoarseness, stridor, or a brassy cough. If already significantly symptomatic, an anesthesiologist with specialized equipment for difficult airways as well as a surgeon should be on standby. Endotracheal intubation and mechanical ventilation are required in the case of respiratory failure. Signs of respiratory failure include the development of tachypnea, use of accessory respiratory muscles, and hypoxemia.
In patients with carbon monoxide (CO) toxicity, pulse oximetry is not adequate for detecting hypoxemia, since the wavelengths for oxyhemoglobin and carboxyhemoglobin are too close together. Pulse oximetry readings would therefore tend to overestimate oxygenation. All patients exposed to smoke in an enclosed space should be screened for CO poisoning by directly measuring a carboxyhemoglobin level with co-oximetry blood gas analysis.
To accurately estimate the depth of skin injury, devitalized tissue must be debrided, and large blisters must be removed. This procedure is usually painful and requires potent analgesics. Burn depth is estimated by careful observation of the wound surface.
The extent of total body surface area (TBSA) covered by second or third degree burns has a great impact on the morbidity and mortality and must be estimated. Areas of first degree burns are associated with negligible mortality, so the important components of the TBSA are the areas of second, third, and fourth degree burns. Although time-consuming, the Lund and Browder chart is the most accurate method of determining TBSA. It consists of an anterior and posterior diagram of a patient that is divided into sections that can be colored according to the distribution of the patient's burns. The TBSA of burn is the sum of the colored areas. Different charts are available for different age groups (see figure 1). An alternative to the Lund and Browder chart is the rule of nines. In this method, the body is divided into eleven areas of nine percent each. Each upper extremity is 9%, the anterior and posterior portions of each lower extremity are 9%, the anterior upper and lower portions of torso are 9% each, the posterior upper and lower portions of the torso are 9% each, and the neck and head together is 9%, to give a total of 99%. The perineum makes up the remaining 1%. However, it must be taken into account that the head is relatively larger and the legs relatively smaller in surface area for children compared with adults. A palm of the hand on one side including the area of the digits is approximately 1% of the body surface area and can also be used to estimate the TBSA of burn.
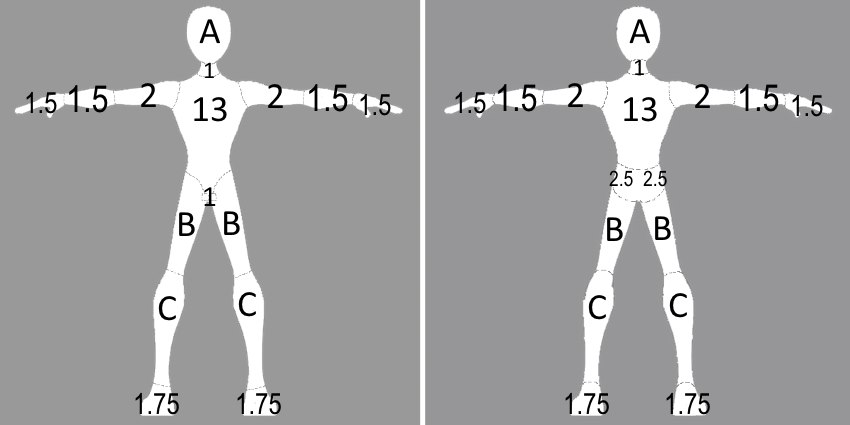
Figure 1. Modified Lund and Browder chart for infants and children using the table values below
Table 1. Burn surface area (%) based on age
A partial thickness burn involving greater than 20% TBSA in any age, greater than 10% in children younger than 10 years old, or a full thickness burn greater than 5% should be hospitalized, preferably in a burn unit where specialized expertise is available. Significant burns of the face, hands, genitalia, feet, or across the joints are categorized as serious. Transfer to or consultation with a burn center should be considered especially for these patients.
Management: Any clothing and jewelry should be removed from the area of the burn. If clothing has adhered to the skin, it should be left for removal during the cleansing of the wound. Non-adherent material may be cut away. To decrease pain, the burn may be cooled with the application of cooled, sterile, saline-soaked gauze.
Prior to cleaning the burn, analgesia is desirable. Burns should be cleansed to remove contaminating debris. Tar or asphalt may be removed with a mixture of cool water and mineral oil. Embedded clothing and debris can be removed by irrigation.
Necrotic tissue must be debrided to minimize infection. Removal of necrotic tissue can be accelerated with the use of enzymatic debriding preparations such as collagenase and papain-urea preparations. These preparations may be less painful and may hasten epithelialization. Blisters that have already lysed should be debrided so that the excess skin does not harbor infection. Flimsy intact large blisters are likely to lyse on their own soon, so these can be debrided as well. Small firm blisters can be left alone. The appearance of the burn on the second day almost always looks worse with enlarging blisters. Parents should be counselled on this so that it can be anticipated appropriately.
Patients suffering wounds deeper than a superficial partial-thickness burn should have their tetanus immunization updated. A topical antibacterial (bacitracin or mupirocin ointment) is not necessary in the treatment of superficial burns but should be used to prevent infection in all other burns. Historically, silver sulfadiazine ointment had been the standard topical medication for the more significant burns, but more recent evidence suggests an increased duration of time for healing compounded by excessive discomfort from the required daily wound dressing changes (5). Once cleansed, the wound should be dressed daily until epithelialization occurs. This will provide some pain relief, protect the wound from infection, and absorb drainage from the wound.
Superficial partial thickness burns heal in approximately 1 to 3 weeks. Most deep partial-thickness burns eventually heal by epithelialization in 3 to 9 weeks. Epithelialization begins in the dermis in the remaining hair follicles. As buds of epithelium grow, they eventually merge to close the wound. Hair follicles are destroyed in full-thickness wounds preventing epithelialization. Full thickness burns require surgical treatment consisting of eschar excision and skin grafting.
Severely injured patients are better served at a designated burn center specifically trained in analgesia and wound care for patients with burns. Transfer to a burn center should be considered with more severe burns, major burns to the hands, face, feet, perineum, or complex electrical burns.
If an extremity is involved, immobilization and elevation may be helpful to reduce edema. Edema may increase ischemia and tissue necrosis. Furthermore, compartment syndrome may develop in an extremity that has sustained a circumferential burn. Patients with circumferential burns of an extremity should be admitted to the hospital for observation of the development of this potentially limb and life threatening condition.
Patients with burns covering 10% to 15% of TBSA or more usually require parenteral fluids. Oral or enteral fluid rehydration may be inadequate in children due to pain, anxiety, and the effects of narcotics. Extravasation of fluid into unburned tissue as well as increased evaporation from the surface of the wound results in hypovolemia. Intravenous or parenteral fluids must be administered to prevent hypovolemia-induced ischemia, lactic acidosis, and shock. Fluid resuscitation with Ringer's lactate or normal saline solution should be administered according to the Parkland formula. This formula estimates the fluid requirements burn patients for the first 24 hours: 4 cc/kg for each TBSA percentage point infused over 24 hours in addition to the maintenance calculation (4). However, urinary output is the best indicator of satisfactory hydration. Although adequate fluid administration is essential, it is important to avoid over-hydration. Increased hydrostatic pressure and decreased oncotic pressure from protein loss contributes to the fluid shift, and over-hydration may result in increased wound and whole-body edema (including pulmonary edema and respiratory compromise).
When administering fluid to infants, it is important to appreciate the lack of maturity of their kidneys. Adult glomerular filtration rate levels are not achieved until 12 months of age and care must be taken to avoid fluid overload while administering fluid infusions adequate to allow for 1 ml/kg/hr of urine output (6).
Loss of water by evaporation leads to heat loss. Small pediatric burn patients are especially at risk for hypothermia. In order to minimize radiant and evaporative heat loss, the ambient temperature should be kept sufficiently high. IV fluids should be warmed during large fluid infusions to prevent iatrogenically induced hypothermia. Special care should be taken in patients younger than 6 months old in this regard. Children in this age group do not have the ability to shiver and can therefore develop profound hypothermia. The basal metabolic rate may double after a major burn injury with caloric requirements rising in proportion to percentage of BSA burned, up to approximately 50% TBSA. Nutritional needs should be carefully assessed and appropriately managed (3).
Most children sustain electrical burns by the insertion of a metal object into a wall outlet or by exposure to frayed electric cords. Intense heat and deep injuries are produced when the current passes through the tissues. If a child puts a live electric cord into the oral cavity, the lips may be burned. Additionally, the burn may extend completely through the lips and oral mucosa to the labial artery. This can be potentially catastrophic if this artery erodes due to sloughing of necrotic tissue. Sudden hemorrhage can occur as late as one week after injury (7).
Burn injuries may result in scarring and contracture. There is a high risk of scar formation associated with burn wounds that take more than 3 weeks to heal. Furthermore, scars may develop in wounds that heal spontaneously without skin grafting. Children tend to scar worse than adults, and patients with dark skin color scar worse than patients with light skin. Pressure garments worn 24 hours a day continuously for one year after healing may limit the progression of scarring. Joint contractures are characteristic of scarring.
Physical and occupational therapy should begin on the day of admission in order to maximize the cosmetic and functional outcome. If necessary, therapy may continue after discharge for several months as the scar tissue forms and contractures develop. Rehabilitation involves joint positioning, active and passive range of motion exercises, limitation of pressure necrosis, ambulation, and assistance in daily activity. Rehabilitation programs for burn patients consist not only of physical support, but emotional support as well. As the pediatric burn patient matures and enters into new social situations, psychological support may be beneficial.
Questions
1. True/False: Antibacterial ointment is indicated for all burns regardless of depth of injury.
2. When treating burns in infants and young children, special considerations include:
. . . . . A. Idiosyncratic injuries
. . . . . B. Excessive heat loss
. . . . . C. Disproportionate body surface areas
. . . . . D. Worsening scar formation
. . . . . E. All of the above
3. When should a patient be sent to a burn unit?
4. A 2 year old toddler has scald burns to the buttocks, both feet (plantar and dorsal sides), and posterior lower extremities. What is the % TBSA?
5. The patient in question 4 weighs 13 kg. What intravenous fluid infusion rate (ml/hr) is needed for the first 24 hrs?
6. Despite following the above fluid formula, a burn patient has a continuous urine output via urinary catheter of only 0.2 ml/kg/hr (ideally, this should be about 1 ml/kg/hr). The child appears to be moderately edemaous. Should the fluid rate be increased or continued at the same rate?
References
1. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control: Data and Statistics (WISQARS) http://www.cdc.gov/injury/wisqars/facts.html (Accessed on March 21, 2013)
2. Hansbrough JF, Hansbrough W. Pediatric Burns. Pediatr Rev 1999;20(4):117-123.
3. Smith ML. Pediatric burns: management of thermal, electrical, and chemical burns and burn-like dermatologic conditions. Pediatr Ann 2000;29(6):367-378.
4. Reed JL, Pomerantz WJ. Emergency management of pediatric burns. Pediatr Emerg Care. 2005 Feb;21(2):118-29.
5. Wasiak J, Cleland H, Campbell F, Spinks A. Dressings for superficial and partial thickness burns. Cochrane Database Syst Rev. 2013 Mar 28(3): CD002106. DOI: 10.1002/14651858.CD002106.pub4.
6. Sheridan R. Burns at the extremes of age. J Burn Care Res. 2007 Jul-Aug;28(4):580-5.
7. Glatstein MM et al. Pediatric Electrical Burn Injuries: Experience of a Large Tertiary Care Hospital and a Review of Electrical Injury. Pediatr Emerg Care. 2013 Jun;29(6):737-40.
Answers to questions
1. False: Antibiotic ointments such as bacitracin or mupirocin ointment do not need to be applied topically for superficial burns; only more serious partial thickness or full thickness burns.
2. E. All of the above including idiosyncratic thermal injuries such as electrical burns to the mouth.
3. A patient should be sent to a burn unit if they have serious burns that are beyond the scope of care in the local institution. Examples of this include, second degree burns of 20% TBSA, third-degree burns of 5% TBSA, major burns to the hands, face, feet, perineum, or electrical burns.
4. 2.5 + 2.5 + 1.75 + 1.75 + 3.75 + 3.75 + 2.5 + 2.5 = 21%
5. Maintenance = 1150 ml over 24 hours = 48 ml/hr. Parkland formula = 21 X 4 = 84 ml/hr. Total infusion rate = 132 ml/hr.
6. The slow urine output indicates hypovolemia. The fluid infusion rate should be increased to improve the urine output.