Child With a Sprained Wrist
Radiology Cases in Pediatric Emergency Medicine
Volume 1, Case 13
Linton L. Yee, MD
Kapiolani Medical Center For Women And Children
University of Hawaii John A. Burns School of Medicine
A ten year old boy fell during a soccer game, injuring
his right wrist. He reportedly tripped when trying to kick
the ball and landed backwards on his outstretched right
hand. After the patient complained of pain and swelling
in the right wrist, ice was placed on his wrist and he
was brought to the ED.
Exam: The right distal wrist is tender with mild
swelling. There is point tenderness over the volar
lateral aspect of the distal radius. There is a mild
amount of loss of range of motion of the right wrist in
flexion, extension, abduction, and adduction. Deformity
and ecchymosis are not present. No tenderness or
deformities are present in the fingers, hand, mid and
proximal forearm, elbow, humerus, shoulder, or clavicle.
Full range of motion is present in the hand, elbow, and
shoulder. There is no tenderness in the anatomic snuff
box. Radiographs of the right wrist are taken.
View radiographs of wrist.
 Clinically, he appears to have a fracture over the
distal radius where there is point tenderness and mild
swelling. Do you see the fracture?
This is normal. No fracture is seen. The growth
plate is not widened, nor is there any displacement of
the epiphysis from the metatphysis. However, this does
not mean that a fracture is ruled out.
Teaching Points:
1. Salter-Harris Type I injuries are based on clinical
suspicion. This is often a clinical diagnosis rather than
a radiographic diagnosis. Tenderness and/or edema at
the growth plate are more diagnostic than normal
radiographic findings. Type I fractures are only visible
radiographically if the segments are displaced;
however, this is uncommon.
View example of displaced SH Type I fracture.
Clinically, he appears to have a fracture over the
distal radius where there is point tenderness and mild
swelling. Do you see the fracture?
This is normal. No fracture is seen. The growth
plate is not widened, nor is there any displacement of
the epiphysis from the metatphysis. However, this does
not mean that a fracture is ruled out.
Teaching Points:
1. Salter-Harris Type I injuries are based on clinical
suspicion. This is often a clinical diagnosis rather than
a radiographic diagnosis. Tenderness and/or edema at
the growth plate are more diagnostic than normal
radiographic findings. Type I fractures are only visible
radiographically if the segments are displaced;
however, this is uncommon.
View example of displaced SH Type I fracture.
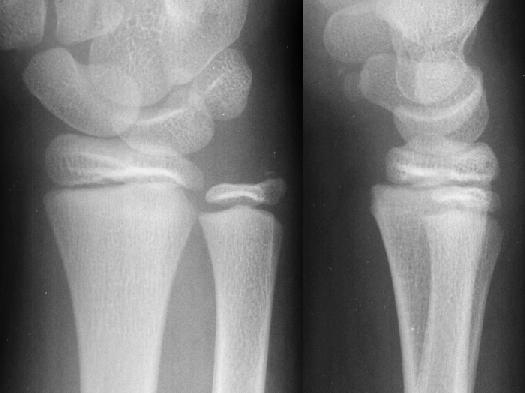
 In this radiograph, the AP view of the wrist looks
normal except for a small chip fracture of the ulnar
styloid. In examining the lateral view, describe the
position of the radial epiphysis in relation to the
metaphysis. Note that the epiphysis is not centered
over the metaphysis. The epiphysis is displaced
dorsally relative to the metaphysis indicating
radiographically, a displaced Salter-Harris Type I
fracture. See Case 18 (Salter-Harris) for more
information.
2. SH Type I fractures of the distal radius are
common. Ulnar involvement is not common.
3. The fall on the outstretched hand is the
mechanism of injury most commonly associated with
fractures of the distal radius and ulna.
4. A sprained wrist is a diagnostic pitfall that should
be avoided. The patient in this case does NOT have a
sprained wrist. Tenderness over the physis region of
any bone, especially at the wrist, is a Salter-Harris I
fracture until proven otherwise by special studies or
long term follow-up, even if initial radiographs are
normal.
5. What might appear to be an ankle sprain may
also turn out to be a SH type I fracture of the distal
fibula. The patient's history may not be very helpful,
since both an ankle sprain and a fibula fracture may be
difficult to distinguish. On examination, a Salter Harris
type I fracture will be tender directly over the distal
fibular physis. An ankle sprain may be tender more
distally where the ligaments/syndesmosis attach the
fibula to the talus. This is a clinical diagnosis as well.
Sometimes, there is evidence of rotation or
displacement of the distal fibular epiphysis, but the
absence of this does not rule out a non-displaced type I
fracture.
View ankle SH-I example.
In this radiograph, the AP view of the wrist looks
normal except for a small chip fracture of the ulnar
styloid. In examining the lateral view, describe the
position of the radial epiphysis in relation to the
metaphysis. Note that the epiphysis is not centered
over the metaphysis. The epiphysis is displaced
dorsally relative to the metaphysis indicating
radiographically, a displaced Salter-Harris Type I
fracture. See Case 18 (Salter-Harris) for more
information.
2. SH Type I fractures of the distal radius are
common. Ulnar involvement is not common.
3. The fall on the outstretched hand is the
mechanism of injury most commonly associated with
fractures of the distal radius and ulna.
4. A sprained wrist is a diagnostic pitfall that should
be avoided. The patient in this case does NOT have a
sprained wrist. Tenderness over the physis region of
any bone, especially at the wrist, is a Salter-Harris I
fracture until proven otherwise by special studies or
long term follow-up, even if initial radiographs are
normal.
5. What might appear to be an ankle sprain may
also turn out to be a SH type I fracture of the distal
fibula. The patient's history may not be very helpful,
since both an ankle sprain and a fibula fracture may be
difficult to distinguish. On examination, a Salter Harris
type I fracture will be tender directly over the distal
fibular physis. An ankle sprain may be tender more
distally where the ligaments/syndesmosis attach the
fibula to the talus. This is a clinical diagnosis as well.
Sometimes, there is evidence of rotation or
displacement of the distal fibular epiphysis, but the
absence of this does not rule out a non-displaced type I
fracture.
View ankle SH-I example.
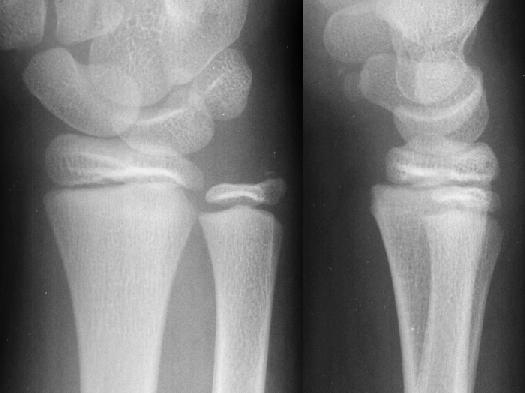
 This patient presented with an ankle injury. He was
noted to have only mild swelling over the lateral
malleolus, but he refused to bear weight on the foot,
preferring to hop instead. He was not tender over the
distal tip of the fibula, but he was very tender more
proximally, over the fibular physis. He was placed in a
splint for a suspected Salter Harris Type I fracture of
the distal fibula. At orthopedic follow-up, he was placed
in a short leg cast for 17 days. Upon removal of the
cast, he had no pain, and he could bear weight without
problems. It is difficult to say with certainty whether this
truly was an SH-I fracture of the distal fibula; however,
this diagnosis should be considered when examination
findings suggest it.
Reference:
1. Lawton LS. Fractures of the Distal Radius and
Ulna. In: Letts RM (ed). Management of Pediatric
Fractures. New York, Churchill Livingstone, Inc.,
1994, pp.345-368.
2. Rang M. Children's Fractures. Philadelphia,
J.B. Lippincott Co., 1983.
3. Anderson AC. Injury-Ankle. In: Fleisher GR,
Ludwig S (eds). Textbook of Pediatric Emergency
Medicine, third edition. Baltimore, Williams & WIlkins,
1993, pp. 259-267.
This patient presented with an ankle injury. He was
noted to have only mild swelling over the lateral
malleolus, but he refused to bear weight on the foot,
preferring to hop instead. He was not tender over the
distal tip of the fibula, but he was very tender more
proximally, over the fibular physis. He was placed in a
splint for a suspected Salter Harris Type I fracture of
the distal fibula. At orthopedic follow-up, he was placed
in a short leg cast for 17 days. Upon removal of the
cast, he had no pain, and he could bear weight without
problems. It is difficult to say with certainty whether this
truly was an SH-I fracture of the distal fibula; however,
this diagnosis should be considered when examination
findings suggest it.
Reference:
1. Lawton LS. Fractures of the Distal Radius and
Ulna. In: Letts RM (ed). Management of Pediatric
Fractures. New York, Churchill Livingstone, Inc.,
1994, pp.345-368.
2. Rang M. Children's Fractures. Philadelphia,
J.B. Lippincott Co., 1983.
3. Anderson AC. Injury-Ankle. In: Fleisher GR,
Ludwig S (eds). Textbook of Pediatric Emergency
Medicine, third edition. Baltimore, Williams & WIlkins,
1993, pp. 259-267.
Return to Radiology Cases In Ped Emerg Med Case Selection Page
Return to Univ. Hawaii Dept. Pediatrics Home Page
 Clinically, he appears to have a fracture over the
distal radius where there is point tenderness and mild
swelling. Do you see the fracture?
This is normal. No fracture is seen. The growth
plate is not widened, nor is there any displacement of
the epiphysis from the metatphysis. However, this does
not mean that a fracture is ruled out.
Teaching Points:
1. Salter-Harris Type I injuries are based on clinical
suspicion. This is often a clinical diagnosis rather than
a radiographic diagnosis. Tenderness and/or edema at
the growth plate are more diagnostic than normal
radiographic findings. Type I fractures are only visible
radiographically if the segments are displaced;
however, this is uncommon.
View example of displaced SH Type I fracture.
Clinically, he appears to have a fracture over the
distal radius where there is point tenderness and mild
swelling. Do you see the fracture?
This is normal. No fracture is seen. The growth
plate is not widened, nor is there any displacement of
the epiphysis from the metatphysis. However, this does
not mean that a fracture is ruled out.
Teaching Points:
1. Salter-Harris Type I injuries are based on clinical
suspicion. This is often a clinical diagnosis rather than
a radiographic diagnosis. Tenderness and/or edema at
the growth plate are more diagnostic than normal
radiographic findings. Type I fractures are only visible
radiographically if the segments are displaced;
however, this is uncommon.
View example of displaced SH Type I fracture.
 In this radiograph, the AP view of the wrist looks
normal except for a small chip fracture of the ulnar
styloid. In examining the lateral view, describe the
position of the radial epiphysis in relation to the
metaphysis. Note that the epiphysis is not centered
over the metaphysis. The epiphysis is displaced
dorsally relative to the metaphysis indicating
radiographically, a displaced Salter-Harris Type I
fracture. See Case 18 (Salter-Harris) for more
information.
2. SH Type I fractures of the distal radius are
common. Ulnar involvement is not common.
3. The fall on the outstretched hand is the
mechanism of injury most commonly associated with
fractures of the distal radius and ulna.
4. A sprained wrist is a diagnostic pitfall that should
be avoided. The patient in this case does NOT have a
sprained wrist. Tenderness over the physis region of
any bone, especially at the wrist, is a Salter-Harris I
fracture until proven otherwise by special studies or
long term follow-up, even if initial radiographs are
normal.
5. What might appear to be an ankle sprain may
also turn out to be a SH type I fracture of the distal
fibula. The patient's history may not be very helpful,
since both an ankle sprain and a fibula fracture may be
difficult to distinguish. On examination, a Salter Harris
type I fracture will be tender directly over the distal
fibular physis. An ankle sprain may be tender more
distally where the ligaments/syndesmosis attach the
fibula to the talus. This is a clinical diagnosis as well.
Sometimes, there is evidence of rotation or
displacement of the distal fibular epiphysis, but the
absence of this does not rule out a non-displaced type I
fracture.
View ankle SH-I example.
In this radiograph, the AP view of the wrist looks
normal except for a small chip fracture of the ulnar
styloid. In examining the lateral view, describe the
position of the radial epiphysis in relation to the
metaphysis. Note that the epiphysis is not centered
over the metaphysis. The epiphysis is displaced
dorsally relative to the metaphysis indicating
radiographically, a displaced Salter-Harris Type I
fracture. See Case 18 (Salter-Harris) for more
information.
2. SH Type I fractures of the distal radius are
common. Ulnar involvement is not common.
3. The fall on the outstretched hand is the
mechanism of injury most commonly associated with
fractures of the distal radius and ulna.
4. A sprained wrist is a diagnostic pitfall that should
be avoided. The patient in this case does NOT have a
sprained wrist. Tenderness over the physis region of
any bone, especially at the wrist, is a Salter-Harris I
fracture until proven otherwise by special studies or
long term follow-up, even if initial radiographs are
normal.
5. What might appear to be an ankle sprain may
also turn out to be a SH type I fracture of the distal
fibula. The patient's history may not be very helpful,
since both an ankle sprain and a fibula fracture may be
difficult to distinguish. On examination, a Salter Harris
type I fracture will be tender directly over the distal
fibular physis. An ankle sprain may be tender more
distally where the ligaments/syndesmosis attach the
fibula to the talus. This is a clinical diagnosis as well.
Sometimes, there is evidence of rotation or
displacement of the distal fibular epiphysis, but the
absence of this does not rule out a non-displaced type I
fracture.
View ankle SH-I example.
 This patient presented with an ankle injury. He was
noted to have only mild swelling over the lateral
malleolus, but he refused to bear weight on the foot,
preferring to hop instead. He was not tender over the
distal tip of the fibula, but he was very tender more
proximally, over the fibular physis. He was placed in a
splint for a suspected Salter Harris Type I fracture of
the distal fibula. At orthopedic follow-up, he was placed
in a short leg cast for 17 days. Upon removal of the
cast, he had no pain, and he could bear weight without
problems. It is difficult to say with certainty whether this
truly was an SH-I fracture of the distal fibula; however,
this diagnosis should be considered when examination
findings suggest it.
Reference:
1. Lawton LS. Fractures of the Distal Radius and
Ulna. In: Letts RM (ed). Management of Pediatric
Fractures. New York, Churchill Livingstone, Inc.,
1994, pp.345-368.
2. Rang M. Children's Fractures. Philadelphia,
J.B. Lippincott Co., 1983.
3. Anderson AC. Injury-Ankle. In: Fleisher GR,
Ludwig S (eds). Textbook of Pediatric Emergency
Medicine, third edition. Baltimore, Williams & WIlkins,
1993, pp. 259-267.
This patient presented with an ankle injury. He was
noted to have only mild swelling over the lateral
malleolus, but he refused to bear weight on the foot,
preferring to hop instead. He was not tender over the
distal tip of the fibula, but he was very tender more
proximally, over the fibular physis. He was placed in a
splint for a suspected Salter Harris Type I fracture of
the distal fibula. At orthopedic follow-up, he was placed
in a short leg cast for 17 days. Upon removal of the
cast, he had no pain, and he could bear weight without
problems. It is difficult to say with certainty whether this
truly was an SH-I fracture of the distal fibula; however,
this diagnosis should be considered when examination
findings suggest it.
Reference:
1. Lawton LS. Fractures of the Distal Radius and
Ulna. In: Letts RM (ed). Management of Pediatric
Fractures. New York, Churchill Livingstone, Inc.,
1994, pp.345-368.
2. Rang M. Children's Fractures. Philadelphia,
J.B. Lippincott Co., 1983.
3. Anderson AC. Injury-Ankle. In: Fleisher GR,
Ludwig S (eds). Textbook of Pediatric Emergency
Medicine, third edition. Baltimore, Williams & WIlkins,
1993, pp. 259-267.