Tachypnea and Abdominal Pain
Radiology Cases in Pediatric Emergency Medicine
Volume 2, Case 5
Loren G. Yamamoto, MD, MPH
Lynette L. Young, MD
Kapiolani Medical Center For Women And Children
University of Hawaii John A. Burns School of Medicine
This is a 6 year old male who was referred from a
rural ED for fever and possible pneumonia. He was
well until three days ago when he was stung by a bee
on his right forearm. He developed a moderate local
reaction with edema and erythema. He saw his primary
care physician the next day at which time he also
complained of chest pain. Chest radiographs were
obtained that day and they were negative. The next
evening (yesterday), he developed fever and worsening
of the swelling and erythema of his right forearm. He
was seen at a rural ED. Cellulitis and a hypersensitivity
reaction were considered. He was placed on oral
cephalexin and acetaminophen with codeine. He took
two doses of cephalexin. He returned to the rural ED in
the morning (today) because of abdominal pain. Chest
radiographs were repeated. This was interpreted as
showing a possible right lower lobe infiltrate. A CBC at
that time showed: WBC 20.4, 67% segs and 18%
bands.
Exam on arrival: VS T38.5 (oral), P145, R44, BP
140/89, oxygen saturation 96% (room air). He was
obese, crying, agitated, and uncooperative, making
examination difficult. HEENT exam significant for
slightly dry oral mucosa. Neck supple. Heart regular,
tachycardic, without murmurs or gallops. Lungs coarse
breath sounds with rhonchi in both bases. Abdominal
guarding noted throughout with tenderness. Bowel
sounds were hypoactive. His right arm was diffusely
indurated and erythematous (difficult to distinguish
cellulitis from hypersensitivity).
He was given a fleets enema for suspected
constipation. He passed large amounts of stool and
seemed to be better in that he was less agitated and
more cooperative. He was noted to be grunting at
times. His abdomen was still tender. More blood
studies were drawn. Radiographs of his chest and
abdomen were obtained.
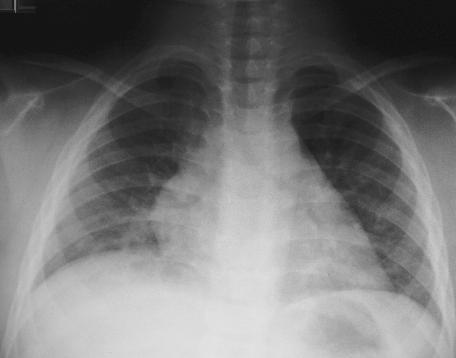
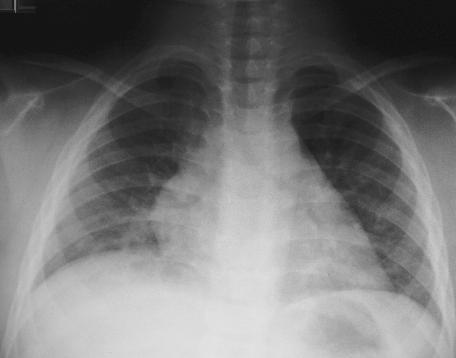
View CXR: PA view.
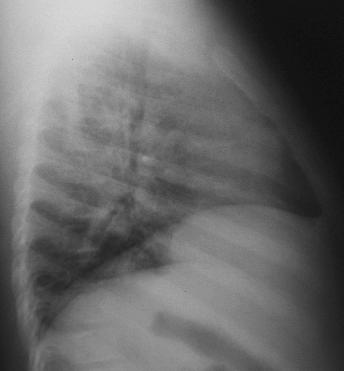
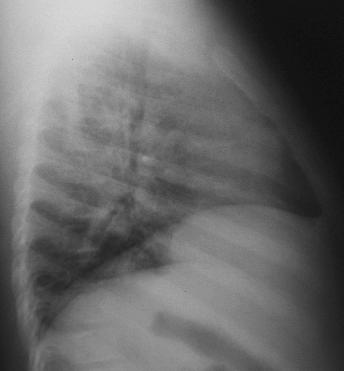
 View CXR: Lateral view.
View CXR: Lateral view.
 View Abdominal Series: Upright view.
View Abdominal Series: Upright view.
 View Abdominal Series: Supine view.
View Abdominal Series: Supine view.
 Although there some subtle abnormalities on his
CXR, there were no definite abnormalities to account
for his grunting and abdominal pain. There were some
possible central infiltrates and the right hemidiaphragm
appeared to be possibly elevated. The inspiratory effort
shown on the film was poor. This was also noted on
the CXR from the rural ED. His abdominal radiographs
showed some bowel distention, but consistent with an
ileus and not a bowel obstruction.
Laboratory results: CBC WBC 33.6, 1 meta, 29
bands, 63 segs, 5 lymphs, 2 monos, Hgb 13.1, Hct
39.0, platelet count 310,000. Na 136, K 4.0, Cl 102,
Bicarb 21, glucose 142. UA SG 1.031, 0-2 WBC,
3-5 RBC.
An abdominal ultrasound was performed looking for
an intra-abdominal abscess. This study showed a
suspicious right lower quadrant mass, but it was unable
to define it further. A surgical consultation was
obtained. The likelihood of acute appendicitis was felt
to be low. A CT scan of the abdomen was obtained.
This study was unremarkable except for a view of the
upper abdomen.
View CT scan.
Although there some subtle abnormalities on his
CXR, there were no definite abnormalities to account
for his grunting and abdominal pain. There were some
possible central infiltrates and the right hemidiaphragm
appeared to be possibly elevated. The inspiratory effort
shown on the film was poor. This was also noted on
the CXR from the rural ED. His abdominal radiographs
showed some bowel distention, but consistent with an
ileus and not a bowel obstruction.
Laboratory results: CBC WBC 33.6, 1 meta, 29
bands, 63 segs, 5 lymphs, 2 monos, Hgb 13.1, Hct
39.0, platelet count 310,000. Na 136, K 4.0, Cl 102,
Bicarb 21, glucose 142. UA SG 1.031, 0-2 WBC,
3-5 RBC.
An abdominal ultrasound was performed looking for
an intra-abdominal abscess. This study showed a
suspicious right lower quadrant mass, but it was unable
to define it further. A surgical consultation was
obtained. The likelihood of acute appendicitis was felt
to be low. A CT scan of the abdomen was obtained.
This study was unremarkable except for a view of the
upper abdomen.
View CT scan.
 This CT cut is through the upper abdomen. It shows
the liver, parts of the diaphragm, and the lower portions
of the lungs. Pulmonary infiltrates are noted in the
posterior portion of the right lower lobe. Note the
pleural effusion adjacent to the infiltrates (arrows). He
was given IV ceftriaxone and hospitalization was
arranged.
Six hours after leaving the ED, house officers
ordered a follow-up CXR (13 hours after the ED CXR,
and 8 hours after the CT scan).
View follow-up CXR.
This CT cut is through the upper abdomen. It shows
the liver, parts of the diaphragm, and the lower portions
of the lungs. Pulmonary infiltrates are noted in the
posterior portion of the right lower lobe. Note the
pleural effusion adjacent to the infiltrates (arrows). He
was given IV ceftriaxone and hospitalization was
arranged.
Six hours after leaving the ED, house officers
ordered a follow-up CXR (13 hours after the ED CXR,
and 8 hours after the CT scan).
View follow-up CXR.
 This CXR shows a large right pleural effusion. This
is a significant change over the 13 hour period since the
previous CXR suggesting a rapidly progressive
pneumonia. This is highly suspicious for a
staphylococcal pneumonia. The source of the staph
was suspected to be the cellulitis on his arm. The
pleural effusion worsened, at which time it was drained
through a tube thoracostomy. Gram stain of the fluid
revealed gram positive cocci. Cell counts 50,000
RBC's, 29,000 WBC's, 70% segs, 18% bands. Protein
5.4 grams/dl, pH 7.0, glucose 8 mg/dl. He required a
second chest tube to drain a loculated empyema.
Other than this, he did remarkably well. He did not
develop any pneumatoceles or a pneumothorax. He
was discharged after 6 weeks of IV antibiotics.
Teaching Points and Discussion
Staphylococcal pneumonia is rapidly progressive in
all age groups. This is a serious pulmonary infection
that is associated with significant morbidity and a high
potential for death.
There are two main forms of staphylococcal
pneumonia. Primary pneumonia is caused by direct
inoculation through the respiratory tract. Secondary or
metastatic hematogenous lung infection is due to
bacteremic seeding of the lung during the course of
endocarditis or septicemia associated with infection at
other sites. It is not unusual to see severe impetigo
associated with staphylococcal pneumonia.
Primary staphylococcal pneumonia is a disease of
infancy and childhood with three-quarters of the cases
involving patients less than one-year old. Predisposing
factors include cystic fibrosis, chronic lung disease,
leukemia, preexisting skin infection, and viral respiratory
infection (measles, influenza, adenovirus).
The patients with staphylococcal pneumonia may
present with fever, lethargy, severe respiratory distress
(tachypnea, grunting, retractions, cyanosis), and
gastrointestinal disturbances (anorexia, vomiting,
abdominal distention). About 75% of patients present
with fever, cough, and dyspnea. The rapid progression
of clinical symptoms is characteristic of staphylococcal
pneumonia.
Chest radiographs in the early stage of
staphylococcal pneumonia may be normal or show a
minimal focal infiltrate. In general, there is a rapid
progression of radiographic findings over just a few
hours. The segmental bronchopneumonia pattern is
usually unilateral and then expands to involve other
lobes. In the case of our patient here, he presented
with abdominal pain and tachypnea. A small infiltrate
was noted which progressed to a large pleural effusion
over a few hours.
About 71% of pneumonias due to Staph aureus
have associated pleural effusions. The effusion is on
the right in 65%, on the left in 15% and bilateral 20% of
the time. This frequently progresses to an empyema.
Ultrasound or CT is often helpful in locating the
loculated fluid.
A pulmonary pneumatocele is a frequent
complication of staphylococcal pneumonia with an
incidence of greater than 85%. There are usually
multiple pneumatoceles which vary in size.
Pneumatoceles are believed to be caused by a partial
airway obstruction by intraluminal exudate or a
peribronchial abscess.
A lung abscess is another complication of
staphylococcal pneumonia. An abscess is a relatively
thick-walled cavity, in contrast to a pneumatocele which
is usually a thin-walled radiolucent area. Fluid levels
may be present in both pneumatoceles and abscesses.
The incidence of pneumothorax associated with
staphylococcal pneumonia is between 40% to 60%. A
pneumothorax may result from a pneumatocele rupture
or formation of a bronchopleural fistula (localized
bronchial wall necrosis). A pyopneumothorax
(pneumothorax + empyema) is highly suggestive of
staphylococcal pneumonia.
Empyemas require drainage with large bore tube
thoracostomies. The empyema is often rapidly
progressive, which leads to compression of the lung
and respiratory failure unless the empyema is drained.
It is likely to reaccumulate following a thoracentesis.
Chest tube thoracostomy also has the benefit of
maintaining lung expansion if a pneumothorax
develops.
A pathogen is recovered from patients with
pneumonia and effusions about 76% of the time. Of
these, pleural fluid cultures are positive in 86% and
blood cultures are positive in 10%.
Although antibiotic coverage with anti-staphylococcal
penicillins (e.g., oxacillin) or first generation
cephalosporins (e.g.. cefazolin) is usually sufficient,
there is a substantial rate of resistance to these drugs.
Methicillin resistant staph aureus will usually be
cephalosporin resistant as well. Vancomycin should be
added to the anti-staphylococcal antibiotic regimen until
sensitivities of the organism are determined.
Complications of staphylococcal pneumonia include
endocarditis, purulent pericarditis, osteomyelitis, deep
tissue abscess, septic arthritis, and meningitis.
References
Chartrand SA, McCracken GH. Staphylococcal
pneumonia in infants and children. Ped Infect Dis
1982;1:19-23.
Forbes GB, Emerson GL. Staphylococcal
pneumonia and empyema. Pediat Clin N Amer
1957;4:215-229.
Melish ME. Staphylococcal Infections. In: Feigin
RD, Cherry JD (eds). Textbook of Pediatric Infectious
Diseases, 2nd edition, 1987, Philadelphia, WB
Saunders Company, pp. 1260-1292.
This CXR shows a large right pleural effusion. This
is a significant change over the 13 hour period since the
previous CXR suggesting a rapidly progressive
pneumonia. This is highly suspicious for a
staphylococcal pneumonia. The source of the staph
was suspected to be the cellulitis on his arm. The
pleural effusion worsened, at which time it was drained
through a tube thoracostomy. Gram stain of the fluid
revealed gram positive cocci. Cell counts 50,000
RBC's, 29,000 WBC's, 70% segs, 18% bands. Protein
5.4 grams/dl, pH 7.0, glucose 8 mg/dl. He required a
second chest tube to drain a loculated empyema.
Other than this, he did remarkably well. He did not
develop any pneumatoceles or a pneumothorax. He
was discharged after 6 weeks of IV antibiotics.
Teaching Points and Discussion
Staphylococcal pneumonia is rapidly progressive in
all age groups. This is a serious pulmonary infection
that is associated with significant morbidity and a high
potential for death.
There are two main forms of staphylococcal
pneumonia. Primary pneumonia is caused by direct
inoculation through the respiratory tract. Secondary or
metastatic hematogenous lung infection is due to
bacteremic seeding of the lung during the course of
endocarditis or septicemia associated with infection at
other sites. It is not unusual to see severe impetigo
associated with staphylococcal pneumonia.
Primary staphylococcal pneumonia is a disease of
infancy and childhood with three-quarters of the cases
involving patients less than one-year old. Predisposing
factors include cystic fibrosis, chronic lung disease,
leukemia, preexisting skin infection, and viral respiratory
infection (measles, influenza, adenovirus).
The patients with staphylococcal pneumonia may
present with fever, lethargy, severe respiratory distress
(tachypnea, grunting, retractions, cyanosis), and
gastrointestinal disturbances (anorexia, vomiting,
abdominal distention). About 75% of patients present
with fever, cough, and dyspnea. The rapid progression
of clinical symptoms is characteristic of staphylococcal
pneumonia.
Chest radiographs in the early stage of
staphylococcal pneumonia may be normal or show a
minimal focal infiltrate. In general, there is a rapid
progression of radiographic findings over just a few
hours. The segmental bronchopneumonia pattern is
usually unilateral and then expands to involve other
lobes. In the case of our patient here, he presented
with abdominal pain and tachypnea. A small infiltrate
was noted which progressed to a large pleural effusion
over a few hours.
About 71% of pneumonias due to Staph aureus
have associated pleural effusions. The effusion is on
the right in 65%, on the left in 15% and bilateral 20% of
the time. This frequently progresses to an empyema.
Ultrasound or CT is often helpful in locating the
loculated fluid.
A pulmonary pneumatocele is a frequent
complication of staphylococcal pneumonia with an
incidence of greater than 85%. There are usually
multiple pneumatoceles which vary in size.
Pneumatoceles are believed to be caused by a partial
airway obstruction by intraluminal exudate or a
peribronchial abscess.
A lung abscess is another complication of
staphylococcal pneumonia. An abscess is a relatively
thick-walled cavity, in contrast to a pneumatocele which
is usually a thin-walled radiolucent area. Fluid levels
may be present in both pneumatoceles and abscesses.
The incidence of pneumothorax associated with
staphylococcal pneumonia is between 40% to 60%. A
pneumothorax may result from a pneumatocele rupture
or formation of a bronchopleural fistula (localized
bronchial wall necrosis). A pyopneumothorax
(pneumothorax + empyema) is highly suggestive of
staphylococcal pneumonia.
Empyemas require drainage with large bore tube
thoracostomies. The empyema is often rapidly
progressive, which leads to compression of the lung
and respiratory failure unless the empyema is drained.
It is likely to reaccumulate following a thoracentesis.
Chest tube thoracostomy also has the benefit of
maintaining lung expansion if a pneumothorax
develops.
A pathogen is recovered from patients with
pneumonia and effusions about 76% of the time. Of
these, pleural fluid cultures are positive in 86% and
blood cultures are positive in 10%.
Although antibiotic coverage with anti-staphylococcal
penicillins (e.g., oxacillin) or first generation
cephalosporins (e.g.. cefazolin) is usually sufficient,
there is a substantial rate of resistance to these drugs.
Methicillin resistant staph aureus will usually be
cephalosporin resistant as well. Vancomycin should be
added to the anti-staphylococcal antibiotic regimen until
sensitivities of the organism are determined.
Complications of staphylococcal pneumonia include
endocarditis, purulent pericarditis, osteomyelitis, deep
tissue abscess, septic arthritis, and meningitis.
References
Chartrand SA, McCracken GH. Staphylococcal
pneumonia in infants and children. Ped Infect Dis
1982;1:19-23.
Forbes GB, Emerson GL. Staphylococcal
pneumonia and empyema. Pediat Clin N Amer
1957;4:215-229.
Melish ME. Staphylococcal Infections. In: Feigin
RD, Cherry JD (eds). Textbook of Pediatric Infectious
Diseases, 2nd edition, 1987, Philadelphia, WB
Saunders Company, pp. 1260-1292.
Return to Radiology Cases In Ped Emerg Med Case Selection Page
Return to Univ. Hawaii Dept. Pediatrics Home Page
 View CXR: Lateral view.
View CXR: Lateral view.
 View Abdominal Series: Upright view.
View Abdominal Series: Upright view.
 View Abdominal Series: Supine view.
View Abdominal Series: Supine view.
 Although there some subtle abnormalities on his
CXR, there were no definite abnormalities to account
for his grunting and abdominal pain. There were some
possible central infiltrates and the right hemidiaphragm
appeared to be possibly elevated. The inspiratory effort
shown on the film was poor. This was also noted on
the CXR from the rural ED. His abdominal radiographs
showed some bowel distention, but consistent with an
ileus and not a bowel obstruction.
Laboratory results: CBC WBC 33.6, 1 meta, 29
bands, 63 segs, 5 lymphs, 2 monos, Hgb 13.1, Hct
39.0, platelet count 310,000. Na 136, K 4.0, Cl 102,
Bicarb 21, glucose 142. UA SG 1.031, 0-2 WBC,
3-5 RBC.
An abdominal ultrasound was performed looking for
an intra-abdominal abscess. This study showed a
suspicious right lower quadrant mass, but it was unable
to define it further. A surgical consultation was
obtained. The likelihood of acute appendicitis was felt
to be low. A CT scan of the abdomen was obtained.
This study was unremarkable except for a view of the
upper abdomen.
View CT scan.
Although there some subtle abnormalities on his
CXR, there were no definite abnormalities to account
for his grunting and abdominal pain. There were some
possible central infiltrates and the right hemidiaphragm
appeared to be possibly elevated. The inspiratory effort
shown on the film was poor. This was also noted on
the CXR from the rural ED. His abdominal radiographs
showed some bowel distention, but consistent with an
ileus and not a bowel obstruction.
Laboratory results: CBC WBC 33.6, 1 meta, 29
bands, 63 segs, 5 lymphs, 2 monos, Hgb 13.1, Hct
39.0, platelet count 310,000. Na 136, K 4.0, Cl 102,
Bicarb 21, glucose 142. UA SG 1.031, 0-2 WBC,
3-5 RBC.
An abdominal ultrasound was performed looking for
an intra-abdominal abscess. This study showed a
suspicious right lower quadrant mass, but it was unable
to define it further. A surgical consultation was
obtained. The likelihood of acute appendicitis was felt
to be low. A CT scan of the abdomen was obtained.
This study was unremarkable except for a view of the
upper abdomen.
View CT scan.
 This CT cut is through the upper abdomen. It shows
the liver, parts of the diaphragm, and the lower portions
of the lungs. Pulmonary infiltrates are noted in the
posterior portion of the right lower lobe. Note the
pleural effusion adjacent to the infiltrates (arrows). He
was given IV ceftriaxone and hospitalization was
arranged.
Six hours after leaving the ED, house officers
ordered a follow-up CXR (13 hours after the ED CXR,
and 8 hours after the CT scan).
View follow-up CXR.
This CT cut is through the upper abdomen. It shows
the liver, parts of the diaphragm, and the lower portions
of the lungs. Pulmonary infiltrates are noted in the
posterior portion of the right lower lobe. Note the
pleural effusion adjacent to the infiltrates (arrows). He
was given IV ceftriaxone and hospitalization was
arranged.
Six hours after leaving the ED, house officers
ordered a follow-up CXR (13 hours after the ED CXR,
and 8 hours after the CT scan).
View follow-up CXR.
 This CXR shows a large right pleural effusion. This
is a significant change over the 13 hour period since the
previous CXR suggesting a rapidly progressive
pneumonia. This is highly suspicious for a
staphylococcal pneumonia. The source of the staph
was suspected to be the cellulitis on his arm. The
pleural effusion worsened, at which time it was drained
through a tube thoracostomy. Gram stain of the fluid
revealed gram positive cocci. Cell counts 50,000
RBC's, 29,000 WBC's, 70% segs, 18% bands. Protein
5.4 grams/dl, pH 7.0, glucose 8 mg/dl. He required a
second chest tube to drain a loculated empyema.
Other than this, he did remarkably well. He did not
develop any pneumatoceles or a pneumothorax. He
was discharged after 6 weeks of IV antibiotics.
Teaching Points and Discussion
Staphylococcal pneumonia is rapidly progressive in
all age groups. This is a serious pulmonary infection
that is associated with significant morbidity and a high
potential for death.
There are two main forms of staphylococcal
pneumonia. Primary pneumonia is caused by direct
inoculation through the respiratory tract. Secondary or
metastatic hematogenous lung infection is due to
bacteremic seeding of the lung during the course of
endocarditis or septicemia associated with infection at
other sites. It is not unusual to see severe impetigo
associated with staphylococcal pneumonia.
Primary staphylococcal pneumonia is a disease of
infancy and childhood with three-quarters of the cases
involving patients less than one-year old. Predisposing
factors include cystic fibrosis, chronic lung disease,
leukemia, preexisting skin infection, and viral respiratory
infection (measles, influenza, adenovirus).
The patients with staphylococcal pneumonia may
present with fever, lethargy, severe respiratory distress
(tachypnea, grunting, retractions, cyanosis), and
gastrointestinal disturbances (anorexia, vomiting,
abdominal distention). About 75% of patients present
with fever, cough, and dyspnea. The rapid progression
of clinical symptoms is characteristic of staphylococcal
pneumonia.
Chest radiographs in the early stage of
staphylococcal pneumonia may be normal or show a
minimal focal infiltrate. In general, there is a rapid
progression of radiographic findings over just a few
hours. The segmental bronchopneumonia pattern is
usually unilateral and then expands to involve other
lobes. In the case of our patient here, he presented
with abdominal pain and tachypnea. A small infiltrate
was noted which progressed to a large pleural effusion
over a few hours.
About 71% of pneumonias due to Staph aureus
have associated pleural effusions. The effusion is on
the right in 65%, on the left in 15% and bilateral 20% of
the time. This frequently progresses to an empyema.
Ultrasound or CT is often helpful in locating the
loculated fluid.
A pulmonary pneumatocele is a frequent
complication of staphylococcal pneumonia with an
incidence of greater than 85%. There are usually
multiple pneumatoceles which vary in size.
Pneumatoceles are believed to be caused by a partial
airway obstruction by intraluminal exudate or a
peribronchial abscess.
A lung abscess is another complication of
staphylococcal pneumonia. An abscess is a relatively
thick-walled cavity, in contrast to a pneumatocele which
is usually a thin-walled radiolucent area. Fluid levels
may be present in both pneumatoceles and abscesses.
The incidence of pneumothorax associated with
staphylococcal pneumonia is between 40% to 60%. A
pneumothorax may result from a pneumatocele rupture
or formation of a bronchopleural fistula (localized
bronchial wall necrosis). A pyopneumothorax
(pneumothorax + empyema) is highly suggestive of
staphylococcal pneumonia.
Empyemas require drainage with large bore tube
thoracostomies. The empyema is often rapidly
progressive, which leads to compression of the lung
and respiratory failure unless the empyema is drained.
It is likely to reaccumulate following a thoracentesis.
Chest tube thoracostomy also has the benefit of
maintaining lung expansion if a pneumothorax
develops.
A pathogen is recovered from patients with
pneumonia and effusions about 76% of the time. Of
these, pleural fluid cultures are positive in 86% and
blood cultures are positive in 10%.
Although antibiotic coverage with anti-staphylococcal
penicillins (e.g., oxacillin) or first generation
cephalosporins (e.g.. cefazolin) is usually sufficient,
there is a substantial rate of resistance to these drugs.
Methicillin resistant staph aureus will usually be
cephalosporin resistant as well. Vancomycin should be
added to the anti-staphylococcal antibiotic regimen until
sensitivities of the organism are determined.
Complications of staphylococcal pneumonia include
endocarditis, purulent pericarditis, osteomyelitis, deep
tissue abscess, septic arthritis, and meningitis.
References
Chartrand SA, McCracken GH. Staphylococcal
pneumonia in infants and children. Ped Infect Dis
1982;1:19-23.
Forbes GB, Emerson GL. Staphylococcal
pneumonia and empyema. Pediat Clin N Amer
1957;4:215-229.
Melish ME. Staphylococcal Infections. In: Feigin
RD, Cherry JD (eds). Textbook of Pediatric Infectious
Diseases, 2nd edition, 1987, Philadelphia, WB
Saunders Company, pp. 1260-1292.
This CXR shows a large right pleural effusion. This
is a significant change over the 13 hour period since the
previous CXR suggesting a rapidly progressive
pneumonia. This is highly suspicious for a
staphylococcal pneumonia. The source of the staph
was suspected to be the cellulitis on his arm. The
pleural effusion worsened, at which time it was drained
through a tube thoracostomy. Gram stain of the fluid
revealed gram positive cocci. Cell counts 50,000
RBC's, 29,000 WBC's, 70% segs, 18% bands. Protein
5.4 grams/dl, pH 7.0, glucose 8 mg/dl. He required a
second chest tube to drain a loculated empyema.
Other than this, he did remarkably well. He did not
develop any pneumatoceles or a pneumothorax. He
was discharged after 6 weeks of IV antibiotics.
Teaching Points and Discussion
Staphylococcal pneumonia is rapidly progressive in
all age groups. This is a serious pulmonary infection
that is associated with significant morbidity and a high
potential for death.
There are two main forms of staphylococcal
pneumonia. Primary pneumonia is caused by direct
inoculation through the respiratory tract. Secondary or
metastatic hematogenous lung infection is due to
bacteremic seeding of the lung during the course of
endocarditis or septicemia associated with infection at
other sites. It is not unusual to see severe impetigo
associated with staphylococcal pneumonia.
Primary staphylococcal pneumonia is a disease of
infancy and childhood with three-quarters of the cases
involving patients less than one-year old. Predisposing
factors include cystic fibrosis, chronic lung disease,
leukemia, preexisting skin infection, and viral respiratory
infection (measles, influenza, adenovirus).
The patients with staphylococcal pneumonia may
present with fever, lethargy, severe respiratory distress
(tachypnea, grunting, retractions, cyanosis), and
gastrointestinal disturbances (anorexia, vomiting,
abdominal distention). About 75% of patients present
with fever, cough, and dyspnea. The rapid progression
of clinical symptoms is characteristic of staphylococcal
pneumonia.
Chest radiographs in the early stage of
staphylococcal pneumonia may be normal or show a
minimal focal infiltrate. In general, there is a rapid
progression of radiographic findings over just a few
hours. The segmental bronchopneumonia pattern is
usually unilateral and then expands to involve other
lobes. In the case of our patient here, he presented
with abdominal pain and tachypnea. A small infiltrate
was noted which progressed to a large pleural effusion
over a few hours.
About 71% of pneumonias due to Staph aureus
have associated pleural effusions. The effusion is on
the right in 65%, on the left in 15% and bilateral 20% of
the time. This frequently progresses to an empyema.
Ultrasound or CT is often helpful in locating the
loculated fluid.
A pulmonary pneumatocele is a frequent
complication of staphylococcal pneumonia with an
incidence of greater than 85%. There are usually
multiple pneumatoceles which vary in size.
Pneumatoceles are believed to be caused by a partial
airway obstruction by intraluminal exudate or a
peribronchial abscess.
A lung abscess is another complication of
staphylococcal pneumonia. An abscess is a relatively
thick-walled cavity, in contrast to a pneumatocele which
is usually a thin-walled radiolucent area. Fluid levels
may be present in both pneumatoceles and abscesses.
The incidence of pneumothorax associated with
staphylococcal pneumonia is between 40% to 60%. A
pneumothorax may result from a pneumatocele rupture
or formation of a bronchopleural fistula (localized
bronchial wall necrosis). A pyopneumothorax
(pneumothorax + empyema) is highly suggestive of
staphylococcal pneumonia.
Empyemas require drainage with large bore tube
thoracostomies. The empyema is often rapidly
progressive, which leads to compression of the lung
and respiratory failure unless the empyema is drained.
It is likely to reaccumulate following a thoracentesis.
Chest tube thoracostomy also has the benefit of
maintaining lung expansion if a pneumothorax
develops.
A pathogen is recovered from patients with
pneumonia and effusions about 76% of the time. Of
these, pleural fluid cultures are positive in 86% and
blood cultures are positive in 10%.
Although antibiotic coverage with anti-staphylococcal
penicillins (e.g., oxacillin) or first generation
cephalosporins (e.g.. cefazolin) is usually sufficient,
there is a substantial rate of resistance to these drugs.
Methicillin resistant staph aureus will usually be
cephalosporin resistant as well. Vancomycin should be
added to the anti-staphylococcal antibiotic regimen until
sensitivities of the organism are determined.
Complications of staphylococcal pneumonia include
endocarditis, purulent pericarditis, osteomyelitis, deep
tissue abscess, septic arthritis, and meningitis.
References
Chartrand SA, McCracken GH. Staphylococcal
pneumonia in infants and children. Ped Infect Dis
1982;1:19-23.
Forbes GB, Emerson GL. Staphylococcal
pneumonia and empyema. Pediat Clin N Amer
1957;4:215-229.
Melish ME. Staphylococcal Infections. In: Feigin
RD, Cherry JD (eds). Textbook of Pediatric Infectious
Diseases, 2nd edition, 1987, Philadelphia, WB
Saunders Company, pp. 1260-1292.