Recurrent Pneumonia
Radiology Cases in Pediatric Emergency Medicine
Volume 2, Case 7
Andrew K. Feng, MD
Kapiolani Medical Center For Women And Children
University of Hawaii John A. Burns School of Medicine
This is a two-year old Caucasian male with a chief
complaint of cough and fever. He has had fevers up to
38.5 degrees and "wet" coughs intermittently for the
past two months. He has also had episodes of emesis
and decreased activity. His initial diagnosis had been
"bronchitis," which was empirically treated with an oral
cephalosporin. His symptoms improved somewhat, but
later recurred. At that time, a chest radiograph (CXR)
revealed a right lower lobe infiltrate, and he was then
treated with erythromycin/sulfamethoxazole. Again, his
symptoms initially improved but recurred within two
days.
After being ill for one month, he was hospitalized for
recurrent and persistent pneumonia with a suspected
foreign body in the right mainstem bronchus on CXR.
In retrospect, his mother recalls the child choking on
almonds prior to the initial onset of symptoms. A
bronchoscopy was performed which resulted in removal
of granulation tissue, after which he was treated with
cephalosporins for seven days with improvement.
One week later, he again developed mild
respiratory symptoms and was started empirically on a
different cephalosporin, but his symptoms actually
worsened over the next day. Tuberculin skin testing
and sweat chloride tests were negative. Neonatal
and developmental histories are unremarkable.
Exam VS T39.4 (oral), P164, R36, BP 127/96,
oxygen saturation 98% in room air. He is awake, alert,
consolable, and in no acute distress. HEENT and neck
exams are normal. Heart regular without murmurs.
Lung exam reveals diffuse coarse rhonchi and slightly
diminished breath sounds in the right base, but
otherwise no retractions, wheezing, or rales. The
remainder of his exam is unremarkable.
Another CXR is obtained.
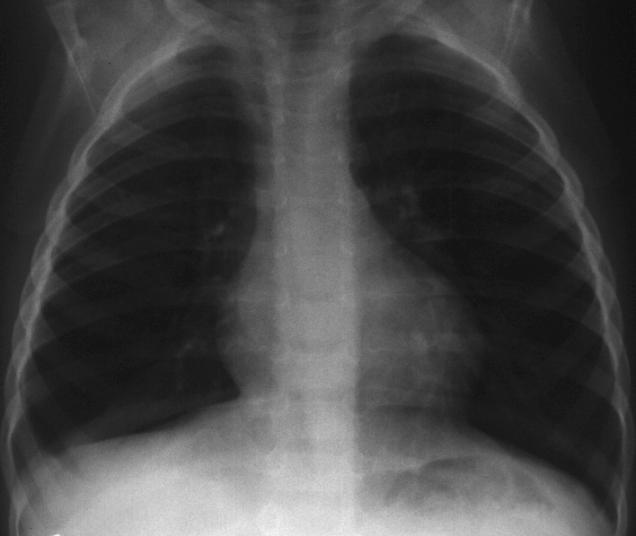
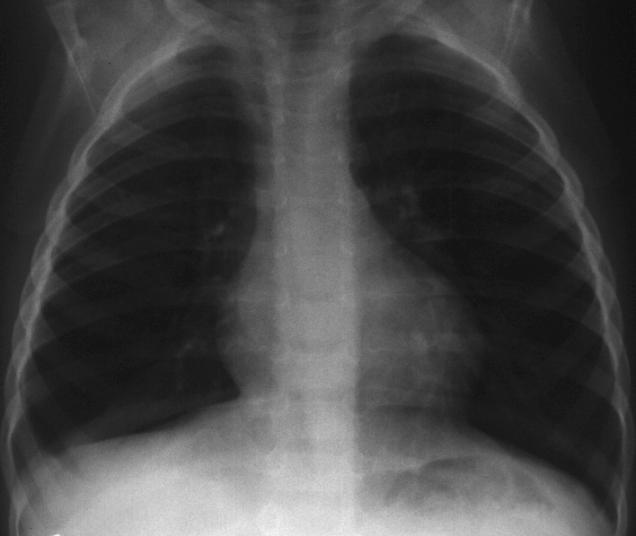
View CXR PA view.
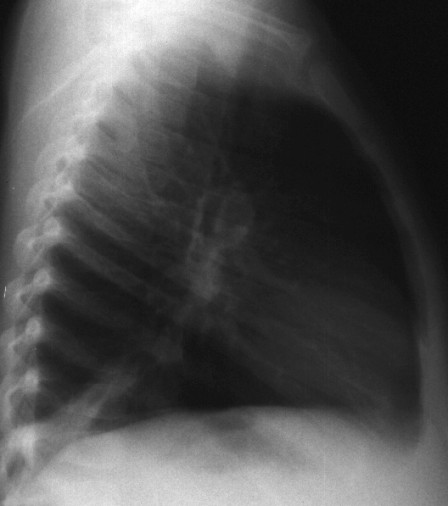
 Lateral view.
Lateral view.
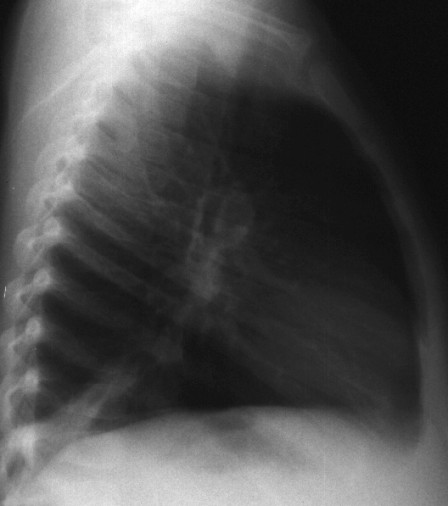 There is moderate subsegmental atelectasis versus
an infiltrate in the right lower lobe. This is best seen
on the lateral view as a linear density in the posterior
lower lung. It is also seen faintly on the PA view in the
right lower lung field, but the scanner was not able to
capture it very well. What would you do at this point?
He has had several pneumonias following a history of
choking on almonds, but a previous bronchoscopy was
negative.
Remember the "principle" discussed in Case 8 of
Volume 1, Foreign Body Aspiration in a Child:
Nuts + Choking = Bronchoscopy
Despite the negative previous bronchoscopy, a
different surgeon is called for bronchoscopy under
general anesthesia. Initial laryngoscopic exam reveals
an erythematous and mildly edematous epiglottis. The
remainder of the procedure is then performed via
bronchoscopy, which reveals an erythematous trachea
with an injected mucosa. There is also moderate
edema in both mainstem bronchi, and marked edema in
the subsegmental bronchi on the right side. The lower
lobe bronchus contains granulation tissue that is friable,
and upon retracting the granulation tissue, a foreign
body is visualized and removed. Histologic exam
reveals vegetable matter consistent with a nut.
Teaching Points and Discussion
Although foreign body aspiration may not be the
most common cause of recurrent pneumonia, it is not
uncommon especially in this age group which varies
from six month olds to three year olds with a peak
incidence at two years of age and a ninety percent
incidence before five years of age (1,2). It is, therefore,
imperative to maintain a high index of suspicion even if
there is no definite history of a choking episode, which
is usually the case in about half the cases, but up to
70% of the time in one study (3).
Most commonly, patients may present with localized
wheezing, diminished air movement, and rhonchi on
auscultation of the lungs. However, these findings may
not always be present and certainly may seem diffuse
over both lung fields due to transmission of those
sounds through the bronchi. Pneumonia may also be a
concomitant finding in up to 20% of the cases.
Recurrent pneumonia may develop secondary to a
foreign body that is obstructing the normal mucociliary
clearance mechanism (4). In fact, there have been
cases of months to even years where an aspirated
foreign body had been the cause of recurrent
pneumonia (5).
More common types of aspirated objects include
peanuts (up to 50% of total cases), raisins, sunflower
seeds, popcorn, teeth, and toys. Foreign body
aspiration should always be considered in a child with
unexplained pulmonary problems.
Evaluation for a foreign body aspiration should
include inspiratory and expiratory CXR's (or bilateral
decubitus CXR's for infants and toddlers who cannot
follow commands) looking for asymmetric air-trapping
secondary to bronchial obstruction. CXR under
fluoroscopy may also aid in detecting diminished
lung/diaphragm movement. A single CXR may detect
the foreign body, but one study demonstrated only four
percent of pulmonary foreign bodies to be radiopaque
(6). Even if all radiographic studies are negative,
clinical suspicion should lead one to consider
bronchoscopy since negative radiographic studies are
not able to totally rule out foreign bodies.
The treatment of choice is bronchoscopy for removal
of the foreign body. Without such removal,
complications may arise such as recurrent pneumonia
(even migratory), pulmonary abscess and/or cyst
development, bronchospasm, pneumothorax and
bronchopleural fistula (5,7).
The differential diagnosis for recurrent pneumonia
can be extensive with the most common etiologies
being reactive airway disease, various
immunodeficiencies, tuberculosis, cystic fibrosis, and
anatomical anomalies (8). In this case, a "choking"
episode while eating nuts was eventually elicited by
history, and repeated pulmonary infiltrates on CXR as
well as localized lung findings on exam suggested a
retained pulmonary foreign body, after which the
appropriate therapy was performed, and the patient's
symptoms eventually resolved.
References
1. Wiseman NE. The Diagnosis of Foreign Body
Aspiration. J Ped Surg 1984;19:531-535.
2. Oski FA (ed). Principles and Practice of
Pediatrics, 2nd Edition. Philadelphia, J.B. Lippincott
Co., 1994, pp. 822, 1475-1477.
3. Moazam F. Foreign Bodies in the Pediatric
Tracheobronchial Tree. Clin Pediatr 1983;22:148.
4. Rubin BK. The Evaluation of the Child with
Recurrent Chest Infections. Pediatr Inf Dis
1985;4(1):88-98.
5. Ben-Dov I. Foreign Body Aspiration in the Adult:
An Occult Cause of Chronic Pulmonary Symptoms.
Postgrad Med J 1989;65(763):299-301.
6. Blazer S. Foreign Body in the Airway: A Review
of 200 Cases. Am J Dis Child 1980;134:68.
7. Barlett JG. The Triple Threat of Aspiration
Pneumonia. Chest 1975;68:560-566.
8. Stockman JA (ed). Difficult Diagnosis in
Pediatrics. Philadelphia, W.B. Saunders Co., 1990,
pp. 375-382.
There is moderate subsegmental atelectasis versus
an infiltrate in the right lower lobe. This is best seen
on the lateral view as a linear density in the posterior
lower lung. It is also seen faintly on the PA view in the
right lower lung field, but the scanner was not able to
capture it very well. What would you do at this point?
He has had several pneumonias following a history of
choking on almonds, but a previous bronchoscopy was
negative.
Remember the "principle" discussed in Case 8 of
Volume 1, Foreign Body Aspiration in a Child:
Nuts + Choking = Bronchoscopy
Despite the negative previous bronchoscopy, a
different surgeon is called for bronchoscopy under
general anesthesia. Initial laryngoscopic exam reveals
an erythematous and mildly edematous epiglottis. The
remainder of the procedure is then performed via
bronchoscopy, which reveals an erythematous trachea
with an injected mucosa. There is also moderate
edema in both mainstem bronchi, and marked edema in
the subsegmental bronchi on the right side. The lower
lobe bronchus contains granulation tissue that is friable,
and upon retracting the granulation tissue, a foreign
body is visualized and removed. Histologic exam
reveals vegetable matter consistent with a nut.
Teaching Points and Discussion
Although foreign body aspiration may not be the
most common cause of recurrent pneumonia, it is not
uncommon especially in this age group which varies
from six month olds to three year olds with a peak
incidence at two years of age and a ninety percent
incidence before five years of age (1,2). It is, therefore,
imperative to maintain a high index of suspicion even if
there is no definite history of a choking episode, which
is usually the case in about half the cases, but up to
70% of the time in one study (3).
Most commonly, patients may present with localized
wheezing, diminished air movement, and rhonchi on
auscultation of the lungs. However, these findings may
not always be present and certainly may seem diffuse
over both lung fields due to transmission of those
sounds through the bronchi. Pneumonia may also be a
concomitant finding in up to 20% of the cases.
Recurrent pneumonia may develop secondary to a
foreign body that is obstructing the normal mucociliary
clearance mechanism (4). In fact, there have been
cases of months to even years where an aspirated
foreign body had been the cause of recurrent
pneumonia (5).
More common types of aspirated objects include
peanuts (up to 50% of total cases), raisins, sunflower
seeds, popcorn, teeth, and toys. Foreign body
aspiration should always be considered in a child with
unexplained pulmonary problems.
Evaluation for a foreign body aspiration should
include inspiratory and expiratory CXR's (or bilateral
decubitus CXR's for infants and toddlers who cannot
follow commands) looking for asymmetric air-trapping
secondary to bronchial obstruction. CXR under
fluoroscopy may also aid in detecting diminished
lung/diaphragm movement. A single CXR may detect
the foreign body, but one study demonstrated only four
percent of pulmonary foreign bodies to be radiopaque
(6). Even if all radiographic studies are negative,
clinical suspicion should lead one to consider
bronchoscopy since negative radiographic studies are
not able to totally rule out foreign bodies.
The treatment of choice is bronchoscopy for removal
of the foreign body. Without such removal,
complications may arise such as recurrent pneumonia
(even migratory), pulmonary abscess and/or cyst
development, bronchospasm, pneumothorax and
bronchopleural fistula (5,7).
The differential diagnosis for recurrent pneumonia
can be extensive with the most common etiologies
being reactive airway disease, various
immunodeficiencies, tuberculosis, cystic fibrosis, and
anatomical anomalies (8). In this case, a "choking"
episode while eating nuts was eventually elicited by
history, and repeated pulmonary infiltrates on CXR as
well as localized lung findings on exam suggested a
retained pulmonary foreign body, after which the
appropriate therapy was performed, and the patient's
symptoms eventually resolved.
References
1. Wiseman NE. The Diagnosis of Foreign Body
Aspiration. J Ped Surg 1984;19:531-535.
2. Oski FA (ed). Principles and Practice of
Pediatrics, 2nd Edition. Philadelphia, J.B. Lippincott
Co., 1994, pp. 822, 1475-1477.
3. Moazam F. Foreign Bodies in the Pediatric
Tracheobronchial Tree. Clin Pediatr 1983;22:148.
4. Rubin BK. The Evaluation of the Child with
Recurrent Chest Infections. Pediatr Inf Dis
1985;4(1):88-98.
5. Ben-Dov I. Foreign Body Aspiration in the Adult:
An Occult Cause of Chronic Pulmonary Symptoms.
Postgrad Med J 1989;65(763):299-301.
6. Blazer S. Foreign Body in the Airway: A Review
of 200 Cases. Am J Dis Child 1980;134:68.
7. Barlett JG. The Triple Threat of Aspiration
Pneumonia. Chest 1975;68:560-566.
8. Stockman JA (ed). Difficult Diagnosis in
Pediatrics. Philadelphia, W.B. Saunders Co., 1990,
pp. 375-382.
Return to Radiology Cases In Ped Emerg Med Case Selection Page
Return to Univ. Hawaii Dept. Pediatrics Home Page
 Lateral view.
Lateral view.
 There is moderate subsegmental atelectasis versus
an infiltrate in the right lower lobe. This is best seen
on the lateral view as a linear density in the posterior
lower lung. It is also seen faintly on the PA view in the
right lower lung field, but the scanner was not able to
capture it very well. What would you do at this point?
He has had several pneumonias following a history of
choking on almonds, but a previous bronchoscopy was
negative.
Remember the "principle" discussed in Case 8 of
Volume 1, Foreign Body Aspiration in a Child:
Nuts + Choking = Bronchoscopy
Despite the negative previous bronchoscopy, a
different surgeon is called for bronchoscopy under
general anesthesia. Initial laryngoscopic exam reveals
an erythematous and mildly edematous epiglottis. The
remainder of the procedure is then performed via
bronchoscopy, which reveals an erythematous trachea
with an injected mucosa. There is also moderate
edema in both mainstem bronchi, and marked edema in
the subsegmental bronchi on the right side. The lower
lobe bronchus contains granulation tissue that is friable,
and upon retracting the granulation tissue, a foreign
body is visualized and removed. Histologic exam
reveals vegetable matter consistent with a nut.
Teaching Points and Discussion
Although foreign body aspiration may not be the
most common cause of recurrent pneumonia, it is not
uncommon especially in this age group which varies
from six month olds to three year olds with a peak
incidence at two years of age and a ninety percent
incidence before five years of age (1,2). It is, therefore,
imperative to maintain a high index of suspicion even if
there is no definite history of a choking episode, which
is usually the case in about half the cases, but up to
70% of the time in one study (3).
Most commonly, patients may present with localized
wheezing, diminished air movement, and rhonchi on
auscultation of the lungs. However, these findings may
not always be present and certainly may seem diffuse
over both lung fields due to transmission of those
sounds through the bronchi. Pneumonia may also be a
concomitant finding in up to 20% of the cases.
Recurrent pneumonia may develop secondary to a
foreign body that is obstructing the normal mucociliary
clearance mechanism (4). In fact, there have been
cases of months to even years where an aspirated
foreign body had been the cause of recurrent
pneumonia (5).
More common types of aspirated objects include
peanuts (up to 50% of total cases), raisins, sunflower
seeds, popcorn, teeth, and toys. Foreign body
aspiration should always be considered in a child with
unexplained pulmonary problems.
Evaluation for a foreign body aspiration should
include inspiratory and expiratory CXR's (or bilateral
decubitus CXR's for infants and toddlers who cannot
follow commands) looking for asymmetric air-trapping
secondary to bronchial obstruction. CXR under
fluoroscopy may also aid in detecting diminished
lung/diaphragm movement. A single CXR may detect
the foreign body, but one study demonstrated only four
percent of pulmonary foreign bodies to be radiopaque
(6). Even if all radiographic studies are negative,
clinical suspicion should lead one to consider
bronchoscopy since negative radiographic studies are
not able to totally rule out foreign bodies.
The treatment of choice is bronchoscopy for removal
of the foreign body. Without such removal,
complications may arise such as recurrent pneumonia
(even migratory), pulmonary abscess and/or cyst
development, bronchospasm, pneumothorax and
bronchopleural fistula (5,7).
The differential diagnosis for recurrent pneumonia
can be extensive with the most common etiologies
being reactive airway disease, various
immunodeficiencies, tuberculosis, cystic fibrosis, and
anatomical anomalies (8). In this case, a "choking"
episode while eating nuts was eventually elicited by
history, and repeated pulmonary infiltrates on CXR as
well as localized lung findings on exam suggested a
retained pulmonary foreign body, after which the
appropriate therapy was performed, and the patient's
symptoms eventually resolved.
References
1. Wiseman NE. The Diagnosis of Foreign Body
Aspiration. J Ped Surg 1984;19:531-535.
2. Oski FA (ed). Principles and Practice of
Pediatrics, 2nd Edition. Philadelphia, J.B. Lippincott
Co., 1994, pp. 822, 1475-1477.
3. Moazam F. Foreign Bodies in the Pediatric
Tracheobronchial Tree. Clin Pediatr 1983;22:148.
4. Rubin BK. The Evaluation of the Child with
Recurrent Chest Infections. Pediatr Inf Dis
1985;4(1):88-98.
5. Ben-Dov I. Foreign Body Aspiration in the Adult:
An Occult Cause of Chronic Pulmonary Symptoms.
Postgrad Med J 1989;65(763):299-301.
6. Blazer S. Foreign Body in the Airway: A Review
of 200 Cases. Am J Dis Child 1980;134:68.
7. Barlett JG. The Triple Threat of Aspiration
Pneumonia. Chest 1975;68:560-566.
8. Stockman JA (ed). Difficult Diagnosis in
Pediatrics. Philadelphia, W.B. Saunders Co., 1990,
pp. 375-382.
There is moderate subsegmental atelectasis versus
an infiltrate in the right lower lobe. This is best seen
on the lateral view as a linear density in the posterior
lower lung. It is also seen faintly on the PA view in the
right lower lung field, but the scanner was not able to
capture it very well. What would you do at this point?
He has had several pneumonias following a history of
choking on almonds, but a previous bronchoscopy was
negative.
Remember the "principle" discussed in Case 8 of
Volume 1, Foreign Body Aspiration in a Child:
Nuts + Choking = Bronchoscopy
Despite the negative previous bronchoscopy, a
different surgeon is called for bronchoscopy under
general anesthesia. Initial laryngoscopic exam reveals
an erythematous and mildly edematous epiglottis. The
remainder of the procedure is then performed via
bronchoscopy, which reveals an erythematous trachea
with an injected mucosa. There is also moderate
edema in both mainstem bronchi, and marked edema in
the subsegmental bronchi on the right side. The lower
lobe bronchus contains granulation tissue that is friable,
and upon retracting the granulation tissue, a foreign
body is visualized and removed. Histologic exam
reveals vegetable matter consistent with a nut.
Teaching Points and Discussion
Although foreign body aspiration may not be the
most common cause of recurrent pneumonia, it is not
uncommon especially in this age group which varies
from six month olds to three year olds with a peak
incidence at two years of age and a ninety percent
incidence before five years of age (1,2). It is, therefore,
imperative to maintain a high index of suspicion even if
there is no definite history of a choking episode, which
is usually the case in about half the cases, but up to
70% of the time in one study (3).
Most commonly, patients may present with localized
wheezing, diminished air movement, and rhonchi on
auscultation of the lungs. However, these findings may
not always be present and certainly may seem diffuse
over both lung fields due to transmission of those
sounds through the bronchi. Pneumonia may also be a
concomitant finding in up to 20% of the cases.
Recurrent pneumonia may develop secondary to a
foreign body that is obstructing the normal mucociliary
clearance mechanism (4). In fact, there have been
cases of months to even years where an aspirated
foreign body had been the cause of recurrent
pneumonia (5).
More common types of aspirated objects include
peanuts (up to 50% of total cases), raisins, sunflower
seeds, popcorn, teeth, and toys. Foreign body
aspiration should always be considered in a child with
unexplained pulmonary problems.
Evaluation for a foreign body aspiration should
include inspiratory and expiratory CXR's (or bilateral
decubitus CXR's for infants and toddlers who cannot
follow commands) looking for asymmetric air-trapping
secondary to bronchial obstruction. CXR under
fluoroscopy may also aid in detecting diminished
lung/diaphragm movement. A single CXR may detect
the foreign body, but one study demonstrated only four
percent of pulmonary foreign bodies to be radiopaque
(6). Even if all radiographic studies are negative,
clinical suspicion should lead one to consider
bronchoscopy since negative radiographic studies are
not able to totally rule out foreign bodies.
The treatment of choice is bronchoscopy for removal
of the foreign body. Without such removal,
complications may arise such as recurrent pneumonia
(even migratory), pulmonary abscess and/or cyst
development, bronchospasm, pneumothorax and
bronchopleural fistula (5,7).
The differential diagnosis for recurrent pneumonia
can be extensive with the most common etiologies
being reactive airway disease, various
immunodeficiencies, tuberculosis, cystic fibrosis, and
anatomical anomalies (8). In this case, a "choking"
episode while eating nuts was eventually elicited by
history, and repeated pulmonary infiltrates on CXR as
well as localized lung findings on exam suggested a
retained pulmonary foreign body, after which the
appropriate therapy was performed, and the patient's
symptoms eventually resolved.
References
1. Wiseman NE. The Diagnosis of Foreign Body
Aspiration. J Ped Surg 1984;19:531-535.
2. Oski FA (ed). Principles and Practice of
Pediatrics, 2nd Edition. Philadelphia, J.B. Lippincott
Co., 1994, pp. 822, 1475-1477.
3. Moazam F. Foreign Bodies in the Pediatric
Tracheobronchial Tree. Clin Pediatr 1983;22:148.
4. Rubin BK. The Evaluation of the Child with
Recurrent Chest Infections. Pediatr Inf Dis
1985;4(1):88-98.
5. Ben-Dov I. Foreign Body Aspiration in the Adult:
An Occult Cause of Chronic Pulmonary Symptoms.
Postgrad Med J 1989;65(763):299-301.
6. Blazer S. Foreign Body in the Airway: A Review
of 200 Cases. Am J Dis Child 1980;134:68.
7. Barlett JG. The Triple Threat of Aspiration
Pneumonia. Chest 1975;68:560-566.
8. Stockman JA (ed). Difficult Diagnosis in
Pediatrics. Philadelphia, W.B. Saunders Co., 1990,
pp. 375-382.