Recurrent Abdominal Pain and Vomiting in a 7-Year Old
Radiology Cases in Pediatric Emergency Medicine
Volume 2, Case 8
Linda M. Rosen, MD
Loren G. Yamamoto, MD, MPH
Kapiolani Medical Center For Women And Children
University of Hawaii John A. Burns School of Medicine
A 7 year old female is brought to the ED with a chief
complaint of abdominal pain. She vomited once and
feels weak. Emesis occurred about 1 hour after eating
saimin (a local soup/noodle dish, also called ramen)
from a neighborhood lunch/snack truck (a small mom
and pop type business). The pain is worse in the
periumbilical region described as painful and somewhat
intermittent. Her mother stated that this happened to
her in the past and they waited too long before coming
in to the emergency room. During this previous
episode, she was given IV fluids at which point, her
symptoms largely resolved and she went home. Her
mother didn't want her to suffer as much as she did the
last time, so she was brought in early this time, despite
only vomiting once.
Exam VS T36.7, HR 91, RR 24, BP 140/81. She is
uncomfortable, but in no respiratory distress. She is
alert and cooperative. Her oral mucosa is moist and
her eyes are not sunken. Neck supple. Heart regular
without murmurs. Lungs clear. Abdomen flat, soft, and
non-tender. Bowel sounds are active. No masses are
felt. No hernias and no CVA tenderness.
Laboratory studies were drawn and an IV infusion of
Lactated Ringer's was started because this was
indirectly requested by her mother in the description of
her past experience. Additionally, the patient seemed
so disproportionately uncomfortable despite her benign
exam findings and a history suggestive of food
poisoning.
Lab results CBC Hgb 15, Hct 45, WBC 14,000
without a left shift. Na 144, K 3.2, Cl 110, Bicarb 22,
glucose 169. The patient received a total of 400cc of
Ringer's Lactate and a phenergan suppository while in
the E.D. At which time, her abdominal pain resolved.
There was no further vomiting since her initial episode
of emesis prior to arrival. She was not retching and she
was feeling much better. She was sleeping and had to
be awakened to go home. She ambulated briefly but
became grumpy after awakening and wanted her
mother to carry her. Her abdomen was non-tender.
She was discharged with a diagnosis of "Food
Poisoning" with the usual vomiting instructions. She
was instructed to return if worse. You might wonder
why a patient who is ill for only an hour had blood tests
and IV fluids. Call it overkill or instinct. Read on. . .
Six hours after discharge from the E.D. the patient
returns because she it still vomiting, has pain, and feels
her abdomen is distended. She has not had a bowel
movement since a small one early in the morning
before the onset of symptoms. Her mother
administered an enema with only fluid return.
Exam VS T37.0, HR 166, RR 48, BP 88/57, oxygen
saturation 97% in room air. Her exam showed a
distended abdomen, diffuse tenderness (more so
periumbilical without rebound), no stool and no
tenderness on rectal exam with a smear showing
specks of heme positive material. A repeat of her labs
was done. CBC WBC 21,500, 65 segs, 20 bands, Hgb
12.4, Hct 36.4. Na 142, K 3.1, Bicarb 17. Shortly after
arrival she vomited 800cc of yellow fluid. An
abdominal series was ordered.
View abdominal series. Flat (supine) view.
 Left lateral decubitus view.
Left lateral decubitus view.
 This series of radiographs shows a large distended
loop in the RUQ. There are other less dilated loops in
the RLQ. The remainder of the abdomen is relatively
gasless. The lateral decubitus view shows only a few
small air fluid levels and the same distended loops.
A surgical consultation was sought. The patient
received Ringers 500cc and was admitted to the
hospital. She was observed and continued to receive
fluid support but became progressively worse. She
developed a fever and dropped her hemoglobin to 5.3.
At surgery, approximately 24 hours after her initial
presentation, she was found to have malrotation with a
midgut volvulus. The small bowel was infarcted and
necrotic and required removal of her entire small
intestine.
In reviewing this case we see the initial presentation
is entirely nonspecific. However, the rapidity of change
in the patient's vital signs, labs, and requirement for
very aggressive fluid management point to the evolution
of a serious problem. The abdominal radiographs
provided important information that could (should?)
have been acted on sooner. The distended loops and
absence of gas in the other areas of the abdomen in
conjunction with the clinical findings of abdominal
distention and bilious vomiting should raise the
suspicion of a bowel obstruction. Unfortunately in
pediatrics, the radiographic diagnosis of a bowel
obstruction may not be very obvious. The aim (aaiimm)
of this case is to consider the following in the differential
diagnosis of a bowel obstruction using the mnemonic
A-A-I-I-M-M:
Adhesions
Appendicitis
Intussusception
Inguinal hernia
Malrotation
Miscellaneous (Meckel's, tumor, duplication, etc.)
View another abdominal series.
Flat (supine) view.
This series of radiographs shows a large distended
loop in the RUQ. There are other less dilated loops in
the RLQ. The remainder of the abdomen is relatively
gasless. The lateral decubitus view shows only a few
small air fluid levels and the same distended loops.
A surgical consultation was sought. The patient
received Ringers 500cc and was admitted to the
hospital. She was observed and continued to receive
fluid support but became progressively worse. She
developed a fever and dropped her hemoglobin to 5.3.
At surgery, approximately 24 hours after her initial
presentation, she was found to have malrotation with a
midgut volvulus. The small bowel was infarcted and
necrotic and required removal of her entire small
intestine.
In reviewing this case we see the initial presentation
is entirely nonspecific. However, the rapidity of change
in the patient's vital signs, labs, and requirement for
very aggressive fluid management point to the evolution
of a serious problem. The abdominal radiographs
provided important information that could (should?)
have been acted on sooner. The distended loops and
absence of gas in the other areas of the abdomen in
conjunction with the clinical findings of abdominal
distention and bilious vomiting should raise the
suspicion of a bowel obstruction. Unfortunately in
pediatrics, the radiographic diagnosis of a bowel
obstruction may not be very obvious. The aim (aaiimm)
of this case is to consider the following in the differential
diagnosis of a bowel obstruction using the mnemonic
A-A-I-I-M-M:
Adhesions
Appendicitis
Intussusception
Inguinal hernia
Malrotation
Miscellaneous (Meckel's, tumor, duplication, etc.)
View another abdominal series.
Flat (supine) view.
 Upright view.
Upright view.
 Comment on this abdominal series. Can you reach
a diagnosis?
These radiographs show very little bowel gas.
There is a small amount of gas on the left. Otherwise,
the only significant air filled loop that is seen, is located
in the RUQ. These findings are again non-specific, but
they suggest the possibility of a bowel obstruction. This
patient turned out to have a malrotation.
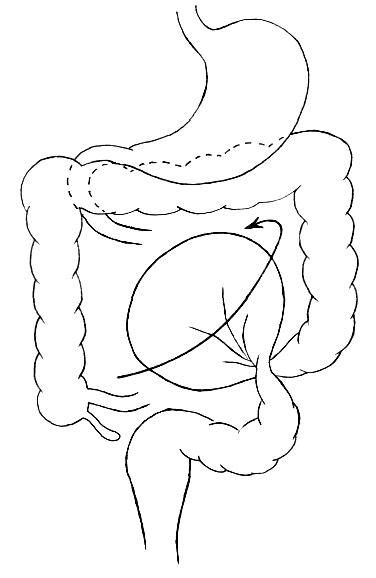
Malrotation of the intestine is the underlying
abnormality which predisposes the bowel to volvulus
(twisting) and subsequent ischemic necrosis. The term
"malrotation" refers to an occurrence in fetal
development at the point where the bowel returns to the
abdominal cavity. After entering the midabdomen
at 12 o'clock, the cecum rotates counterclockwise into
the right lower quadrant at 7 o'clock. The true
significance of the rotation is not so much that the
cecum must be in the right lower quadrant, but the fact
that the mesentery, containing the superior mesenteric
artery, goes with it. The mesentery grows to fix the
terminal ileum to the posterior abdominal wall. This
produces a fan of mesentery securing the small bowel
from the upper midabdomen just behind the duodenum
to the right lower quadrant.
View normal meseteric fixation.
Comment on this abdominal series. Can you reach
a diagnosis?
These radiographs show very little bowel gas.
There is a small amount of gas on the left. Otherwise,
the only significant air filled loop that is seen, is located
in the RUQ. These findings are again non-specific, but
they suggest the possibility of a bowel obstruction. This
patient turned out to have a malrotation.
Malrotation of the intestine is the underlying
abnormality which predisposes the bowel to volvulus
(twisting) and subsequent ischemic necrosis. The term
"malrotation" refers to an occurrence in fetal
development at the point where the bowel returns to the
abdominal cavity. After entering the midabdomen
at 12 o'clock, the cecum rotates counterclockwise into
the right lower quadrant at 7 o'clock. The true
significance of the rotation is not so much that the
cecum must be in the right lower quadrant, but the fact
that the mesentery, containing the superior mesenteric
artery, goes with it. The mesentery grows to fix the
terminal ileum to the posterior abdominal wall. This
produces a fan of mesentery securing the small bowel
from the upper midabdomen just behind the duodenum
to the right lower quadrant.
View normal meseteric fixation.
 Note the broad fan of meseteric attachment of the
small bowel making it difficult for a volvulus of the small
bowel to occur.
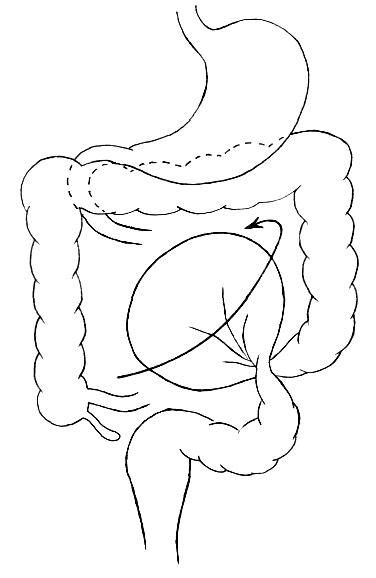
If the correct rotation does not occur, it is termed
"malrotation". This results in the failure of proper
mesenteric development so that instead of a broad fan
of mesenteric attachment, the entire midgut is attached
to the posterior abdominal wall by a short, narrow stalk
in the region of the duodenum. There may also be
bands crossing the duodenum (Ladd's Bands) which
can cause duodenal obstruction.
View malrotation and Ladd's bands.
Note the broad fan of meseteric attachment of the
small bowel making it difficult for a volvulus of the small
bowel to occur.
If the correct rotation does not occur, it is termed
"malrotation". This results in the failure of proper
mesenteric development so that instead of a broad fan
of mesenteric attachment, the entire midgut is attached
to the posterior abdominal wall by a short, narrow stalk
in the region of the duodenum. There may also be
bands crossing the duodenum (Ladd's Bands) which
can cause duodenal obstruction.
View malrotation and Ladd's bands.
 Note the mesenteric attachment of the cecum. This
narrow stalk is more prone to volvulus. Additionally,
this stalk (Ladd's bands) is capable of compressing the
duodenum and obstructing it.
In a malrotation, many meters of intestine are free to
twist around this stalk, which, since it contains the
superior mesenteric artery, is vulnerable to
strangulation and ischemic necrosis. The occurrence of
this twisting and strangulation results in the surgical
emergency called midgut volvulus. Midgut volvulus
should not be confused with cecal or sigmoid volvulus.
Cecal and sigmoid volvulus generally occur in adults.
Sigmoid volvulus involves the large bowel and can often
be decompressed by barium enema or other
non-surgical procedures.
VIew midgut volvulus.
Note the mesenteric attachment of the cecum. This
narrow stalk is more prone to volvulus. Additionally,
this stalk (Ladd's bands) is capable of compressing the
duodenum and obstructing it.
In a malrotation, many meters of intestine are free to
twist around this stalk, which, since it contains the
superior mesenteric artery, is vulnerable to
strangulation and ischemic necrosis. The occurrence of
this twisting and strangulation results in the surgical
emergency called midgut volvulus. Midgut volvulus
should not be confused with cecal or sigmoid volvulus.
Cecal and sigmoid volvulus generally occur in adults.
Sigmoid volvulus involves the large bowel and can often
be decompressed by barium enema or other
non-surgical procedures.
VIew midgut volvulus.
 In midgut volvulus, the majority of the small bowel is
involved in the stragulation. Substantial small bowel
necrosis occurs without prompt surgical intervention.
View cecal volvulus.
In midgut volvulus, the majority of the small bowel is
involved in the stragulation. Substantial small bowel
necrosis occurs without prompt surgical intervention.
View cecal volvulus.
 In malrotation, the cecum may be prone to twisting
or kinking if it is excessively mobile. Cecal volvulus can
occur in the absence of malrotation. This most often
presents in adults rather than children.
View sigmoid volvulus.
In malrotation, the cecum may be prone to twisting
or kinking if it is excessively mobile. Cecal volvulus can
occur in the absence of malrotation. This most often
presents in adults rather than children.
View sigmoid volvulus.
 Sigmoid volvulus is the most common site of colonic
volvulus. It occurs most often in the elderly. It is
associated with elongation of the descending colon
making the sigmoid region hypermobile and prone to
twisting.
Midgut volvulus is a surgical emergency at risk of
bowel infarction. Some neonatal examples of volvulus
are shown below.
View neonatal volvulus case.
Sigmoid volvulus is the most common site of colonic
volvulus. It occurs most often in the elderly. It is
associated with elongation of the descending colon
making the sigmoid region hypermobile and prone to
twisting.
Midgut volvulus is a surgical emergency at risk of
bowel infarction. Some neonatal examples of volvulus
are shown below.
View neonatal volvulus case.
 This radiograph of a 5-day old infant with vomiting
shows a gasless abdomen except for the small air
bubble in the stomach. Such a radiograph should be
considered highly suspicious for any type of upper GI
obstruction. Further studies on this infant showed a
midgut volvulus and malrotation.
View second neonatal case.
This radiograph of a 5-day old infant with vomiting
shows a gasless abdomen except for the small air
bubble in the stomach. Such a radiograph should be
considered highly suspicious for any type of upper GI
obstruction. Further studies on this infant showed a
midgut volvulus and malrotation.
View second neonatal case.
 This radiograph of a 9-day old infant with vomiting
looks relatively normal. It has a normal gas distribution
with no air fluid levels or excessively dilated loops.
Although this radiograph looks much more normal than
the first neonatal radiograph, further studies on this
infant also showed a midgut volvulus and malrotation.
Thus, it is not possible to rule out a volvulus due to
malrotation solely on plain films in some instances.
Clinical suspicion should lead one to pursue more
definitive radiographic studies. While sigmoid
volvulus usually shows severely dilated loops of bowel
and large air fluid levels on plain film radiographs, a
midgut volvulus may show non-specific findings on plain
films without the characteristic signs of an obvious
bowel obstruction.
View BE of second neonatal case.
This radiograph of a 9-day old infant with vomiting
looks relatively normal. It has a normal gas distribution
with no air fluid levels or excessively dilated loops.
Although this radiograph looks much more normal than
the first neonatal radiograph, further studies on this
infant also showed a midgut volvulus and malrotation.
Thus, it is not possible to rule out a volvulus due to
malrotation solely on plain films in some instances.
Clinical suspicion should lead one to pursue more
definitive radiographic studies. While sigmoid
volvulus usually shows severely dilated loops of bowel
and large air fluid levels on plain film radiographs, a
midgut volvulus may show non-specific findings on plain
films without the characteristic signs of an obvious
bowel obstruction.
View BE of second neonatal case.
 This is a barium enema of the infant above
which shows the ascending colon and cecum in the
wrong place. The cecum should normally be located in
the right lower quadrant, but in this BE, most of the
proximal large bowel is in the left upper quadrant. The
cecum is in the central abdomen.
In a patient who has a malrotation but is not
experiencing strangulation, malrotation is usually
identified on an upper GI series or barium enema. The
UGI series can more definitively determine the
presence of malrotation by identifying the position of the
ligament of Treitz. The BE can usually determine the
presence of malrotation by noting the malposition of the
cecum. It should normally be located in the right lower
quadrant. If the cecum is located elsewhere, then
malrotation is likely. However, both of these studies
can be deceiving at times. The ligament of Treitz may
be close to the normal location in a malrotation and the
cecum may occasionally be in the RLQ in a malrotation.
The classic presentation of malrotation is usually
described as a volvulus, heralded by bilious vomiting in
the first days of life. Less than half of the cases
actually present in the neonatal period. Catastrophic
midgut volvulus can present at any age. Lesser
degrees of reversible ischemia (sometimes called
intermittent volvulus), can produce intermittent pain,
non-bilious vomiting, gastroesophageal reflux,
malabsorption and failure to thrive. Patients with
malrotation may be entirely asymptomatic with
catastrophic volvulus occurring at any age. Neither the
age of the patient, nor the chronicity of symptoms are
predictive. All are at risk for severe complications (even
adults). The mortality of midgut volvulus in several
series is 40 to 60%. As some of these series date prior
to modern intensive care techniques, the current
mortality is probably lower, but the survivors may lose
so much bowel that they are totally dependent on
parenteral nutrition. Due to this significant mortality and
morbidity, even incidentally discovered malrotation
should be surgically corrected.
Intestinal obstruction is an uncommon cause of
vomiting in the pediatric age group. Most pediatric
vomiting is caused by infectious agents, including viral
gastroenteritis, but also associated with generalized
non-intestinal infections such as URI, otitis media and
pneumonia. Because of the relative preponderance of
benign causes of vomiting, the serious causes must
always be kept in mind and excluded or at least
anticipated in discharge instructions.
Vomiting in the neonatal period brings to mind
sepsis, congenital anomalies or meconium ileus. In the
first few months of life, pyloric stenosis, hernias and
intussusception are important causes of obstruction.
As the infant becomes mobile, foreign bodies and
poisoning must be considered. Abdominal trauma, both
intentional and accidental can produce vomiting.
In addition to the above, remember A-A-I-I-M-M
(AIM x2). The diagnosis of appendicitis is sometimes
obscure in the young patient. There are no reliable
tests to adequately exclude early appendicitis;
therefore, anticipation of the need for early
reexamination or observation in the emergency
department should be considered in any child with
abdominal pain and vomiting.
References
Powell DM, Othersen HB, Smith CD. Malrotation of
the Intestines in Children: The Effect of Age on
Presentation and Therapy. Journal of Pediatric Surgery
1989;24:777-780.
Andrassy RJ, Mahour GH. Malrotation of the Midgut
in Infants and Children, A 25 Year Review. Archives of
Surgery 1981;116:158-160.
Wang C, Welch CE. Anomalies of Intestinal
Rotation in Adolescents and Adults. Surgery
1963;54:839-855.
Ellenbourg DJ, Delcastillo J. Duodenal Obstruction
From Peritoneal (Ladd's) Bands in a Ten Year Old
Child. Annals of Emergency Medicine 1984;13:56-59.
Schnaufer L, Mahboubi S. Abdominal Emergencies.
In: Fleisher GR, Ludwig S (eds). Textbook of Pediatric
Emergency Medicine, third edition, 1993, Baltimore,
Williams and Wilkins, pp. 1307-1335.
Imbembo AL, Zucker KA. Volvulus of the colon. In:
Sabiston DC (ed). Textbook of Surgery, The Biological
Basis of Modern Surgical Practice, 14th edition.
Philadelphia, W.B. Saunders Company, 199, pp.
940-944.
Smith EI. Malrotation of the intestine. In: Welch
KJ, Randolph JG, Ravitch MM, O'Neill JA, Rowe MI
(eds). Pediatric Surgery, fourth edition. Chicago, Year
Book Medical Publishers, 1986, pp 882-895.
Malrotation. In: Raffensperger JG (ed). Swenson's
Pediatric Surgery, fifth edition. Norwalk, Connecticut,
Appleton & Lange, 1990, pp. 517-522.
This is a barium enema of the infant above
which shows the ascending colon and cecum in the
wrong place. The cecum should normally be located in
the right lower quadrant, but in this BE, most of the
proximal large bowel is in the left upper quadrant. The
cecum is in the central abdomen.
In a patient who has a malrotation but is not
experiencing strangulation, malrotation is usually
identified on an upper GI series or barium enema. The
UGI series can more definitively determine the
presence of malrotation by identifying the position of the
ligament of Treitz. The BE can usually determine the
presence of malrotation by noting the malposition of the
cecum. It should normally be located in the right lower
quadrant. If the cecum is located elsewhere, then
malrotation is likely. However, both of these studies
can be deceiving at times. The ligament of Treitz may
be close to the normal location in a malrotation and the
cecum may occasionally be in the RLQ in a malrotation.
The classic presentation of malrotation is usually
described as a volvulus, heralded by bilious vomiting in
the first days of life. Less than half of the cases
actually present in the neonatal period. Catastrophic
midgut volvulus can present at any age. Lesser
degrees of reversible ischemia (sometimes called
intermittent volvulus), can produce intermittent pain,
non-bilious vomiting, gastroesophageal reflux,
malabsorption and failure to thrive. Patients with
malrotation may be entirely asymptomatic with
catastrophic volvulus occurring at any age. Neither the
age of the patient, nor the chronicity of symptoms are
predictive. All are at risk for severe complications (even
adults). The mortality of midgut volvulus in several
series is 40 to 60%. As some of these series date prior
to modern intensive care techniques, the current
mortality is probably lower, but the survivors may lose
so much bowel that they are totally dependent on
parenteral nutrition. Due to this significant mortality and
morbidity, even incidentally discovered malrotation
should be surgically corrected.
Intestinal obstruction is an uncommon cause of
vomiting in the pediatric age group. Most pediatric
vomiting is caused by infectious agents, including viral
gastroenteritis, but also associated with generalized
non-intestinal infections such as URI, otitis media and
pneumonia. Because of the relative preponderance of
benign causes of vomiting, the serious causes must
always be kept in mind and excluded or at least
anticipated in discharge instructions.
Vomiting in the neonatal period brings to mind
sepsis, congenital anomalies or meconium ileus. In the
first few months of life, pyloric stenosis, hernias and
intussusception are important causes of obstruction.
As the infant becomes mobile, foreign bodies and
poisoning must be considered. Abdominal trauma, both
intentional and accidental can produce vomiting.
In addition to the above, remember A-A-I-I-M-M
(AIM x2). The diagnosis of appendicitis is sometimes
obscure in the young patient. There are no reliable
tests to adequately exclude early appendicitis;
therefore, anticipation of the need for early
reexamination or observation in the emergency
department should be considered in any child with
abdominal pain and vomiting.
References
Powell DM, Othersen HB, Smith CD. Malrotation of
the Intestines in Children: The Effect of Age on
Presentation and Therapy. Journal of Pediatric Surgery
1989;24:777-780.
Andrassy RJ, Mahour GH. Malrotation of the Midgut
in Infants and Children, A 25 Year Review. Archives of
Surgery 1981;116:158-160.
Wang C, Welch CE. Anomalies of Intestinal
Rotation in Adolescents and Adults. Surgery
1963;54:839-855.
Ellenbourg DJ, Delcastillo J. Duodenal Obstruction
From Peritoneal (Ladd's) Bands in a Ten Year Old
Child. Annals of Emergency Medicine 1984;13:56-59.
Schnaufer L, Mahboubi S. Abdominal Emergencies.
In: Fleisher GR, Ludwig S (eds). Textbook of Pediatric
Emergency Medicine, third edition, 1993, Baltimore,
Williams and Wilkins, pp. 1307-1335.
Imbembo AL, Zucker KA. Volvulus of the colon. In:
Sabiston DC (ed). Textbook of Surgery, The Biological
Basis of Modern Surgical Practice, 14th edition.
Philadelphia, W.B. Saunders Company, 199, pp.
940-944.
Smith EI. Malrotation of the intestine. In: Welch
KJ, Randolph JG, Ravitch MM, O'Neill JA, Rowe MI
(eds). Pediatric Surgery, fourth edition. Chicago, Year
Book Medical Publishers, 1986, pp 882-895.
Malrotation. In: Raffensperger JG (ed). Swenson's
Pediatric Surgery, fifth edition. Norwalk, Connecticut,
Appleton & Lange, 1990, pp. 517-522.
Return to Radiology Cases In Ped Emerg Med Case Selection Page
Return to Univ. Hawaii Dept. Pediatrics Home Page
 Left lateral decubitus view.
Left lateral decubitus view.
 This series of radiographs shows a large distended
loop in the RUQ. There are other less dilated loops in
the RLQ. The remainder of the abdomen is relatively
gasless. The lateral decubitus view shows only a few
small air fluid levels and the same distended loops.
A surgical consultation was sought. The patient
received Ringers 500cc and was admitted to the
hospital. She was observed and continued to receive
fluid support but became progressively worse. She
developed a fever and dropped her hemoglobin to 5.3.
At surgery, approximately 24 hours after her initial
presentation, she was found to have malrotation with a
midgut volvulus. The small bowel was infarcted and
necrotic and required removal of her entire small
intestine.
In reviewing this case we see the initial presentation
is entirely nonspecific. However, the rapidity of change
in the patient's vital signs, labs, and requirement for
very aggressive fluid management point to the evolution
of a serious problem. The abdominal radiographs
provided important information that could (should?)
have been acted on sooner. The distended loops and
absence of gas in the other areas of the abdomen in
conjunction with the clinical findings of abdominal
distention and bilious vomiting should raise the
suspicion of a bowel obstruction. Unfortunately in
pediatrics, the radiographic diagnosis of a bowel
obstruction may not be very obvious. The aim (aaiimm)
of this case is to consider the following in the differential
diagnosis of a bowel obstruction using the mnemonic
A-A-I-I-M-M:
Adhesions
Appendicitis
Intussusception
Inguinal hernia
Malrotation
Miscellaneous (Meckel's, tumor, duplication, etc.)
View another abdominal series.
Flat (supine) view.
This series of radiographs shows a large distended
loop in the RUQ. There are other less dilated loops in
the RLQ. The remainder of the abdomen is relatively
gasless. The lateral decubitus view shows only a few
small air fluid levels and the same distended loops.
A surgical consultation was sought. The patient
received Ringers 500cc and was admitted to the
hospital. She was observed and continued to receive
fluid support but became progressively worse. She
developed a fever and dropped her hemoglobin to 5.3.
At surgery, approximately 24 hours after her initial
presentation, she was found to have malrotation with a
midgut volvulus. The small bowel was infarcted and
necrotic and required removal of her entire small
intestine.
In reviewing this case we see the initial presentation
is entirely nonspecific. However, the rapidity of change
in the patient's vital signs, labs, and requirement for
very aggressive fluid management point to the evolution
of a serious problem. The abdominal radiographs
provided important information that could (should?)
have been acted on sooner. The distended loops and
absence of gas in the other areas of the abdomen in
conjunction with the clinical findings of abdominal
distention and bilious vomiting should raise the
suspicion of a bowel obstruction. Unfortunately in
pediatrics, the radiographic diagnosis of a bowel
obstruction may not be very obvious. The aim (aaiimm)
of this case is to consider the following in the differential
diagnosis of a bowel obstruction using the mnemonic
A-A-I-I-M-M:
Adhesions
Appendicitis
Intussusception
Inguinal hernia
Malrotation
Miscellaneous (Meckel's, tumor, duplication, etc.)
View another abdominal series.
Flat (supine) view.
 Upright view.
Upright view.
 Comment on this abdominal series. Can you reach
a diagnosis?
These radiographs show very little bowel gas.
There is a small amount of gas on the left. Otherwise,
the only significant air filled loop that is seen, is located
in the RUQ. These findings are again non-specific, but
they suggest the possibility of a bowel obstruction. This
patient turned out to have a malrotation.
Malrotation of the intestine is the underlying
abnormality which predisposes the bowel to volvulus
(twisting) and subsequent ischemic necrosis. The term
"malrotation" refers to an occurrence in fetal
development at the point where the bowel returns to the
abdominal cavity. After entering the midabdomen
at 12 o'clock, the cecum rotates counterclockwise into
the right lower quadrant at 7 o'clock. The true
significance of the rotation is not so much that the
cecum must be in the right lower quadrant, but the fact
that the mesentery, containing the superior mesenteric
artery, goes with it. The mesentery grows to fix the
terminal ileum to the posterior abdominal wall. This
produces a fan of mesentery securing the small bowel
from the upper midabdomen just behind the duodenum
to the right lower quadrant.
View normal meseteric fixation.
Comment on this abdominal series. Can you reach
a diagnosis?
These radiographs show very little bowel gas.
There is a small amount of gas on the left. Otherwise,
the only significant air filled loop that is seen, is located
in the RUQ. These findings are again non-specific, but
they suggest the possibility of a bowel obstruction. This
patient turned out to have a malrotation.
Malrotation of the intestine is the underlying
abnormality which predisposes the bowel to volvulus
(twisting) and subsequent ischemic necrosis. The term
"malrotation" refers to an occurrence in fetal
development at the point where the bowel returns to the
abdominal cavity. After entering the midabdomen
at 12 o'clock, the cecum rotates counterclockwise into
the right lower quadrant at 7 o'clock. The true
significance of the rotation is not so much that the
cecum must be in the right lower quadrant, but the fact
that the mesentery, containing the superior mesenteric
artery, goes with it. The mesentery grows to fix the
terminal ileum to the posterior abdominal wall. This
produces a fan of mesentery securing the small bowel
from the upper midabdomen just behind the duodenum
to the right lower quadrant.
View normal meseteric fixation.
 Note the broad fan of meseteric attachment of the
small bowel making it difficult for a volvulus of the small
bowel to occur.
If the correct rotation does not occur, it is termed
"malrotation". This results in the failure of proper
mesenteric development so that instead of a broad fan
of mesenteric attachment, the entire midgut is attached
to the posterior abdominal wall by a short, narrow stalk
in the region of the duodenum. There may also be
bands crossing the duodenum (Ladd's Bands) which
can cause duodenal obstruction.
View malrotation and Ladd's bands.
Note the broad fan of meseteric attachment of the
small bowel making it difficult for a volvulus of the small
bowel to occur.
If the correct rotation does not occur, it is termed
"malrotation". This results in the failure of proper
mesenteric development so that instead of a broad fan
of mesenteric attachment, the entire midgut is attached
to the posterior abdominal wall by a short, narrow stalk
in the region of the duodenum. There may also be
bands crossing the duodenum (Ladd's Bands) which
can cause duodenal obstruction.
View malrotation and Ladd's bands.
 Note the mesenteric attachment of the cecum. This
narrow stalk is more prone to volvulus. Additionally,
this stalk (Ladd's bands) is capable of compressing the
duodenum and obstructing it.
In a malrotation, many meters of intestine are free to
twist around this stalk, which, since it contains the
superior mesenteric artery, is vulnerable to
strangulation and ischemic necrosis. The occurrence of
this twisting and strangulation results in the surgical
emergency called midgut volvulus. Midgut volvulus
should not be confused with cecal or sigmoid volvulus.
Cecal and sigmoid volvulus generally occur in adults.
Sigmoid volvulus involves the large bowel and can often
be decompressed by barium enema or other
non-surgical procedures.
VIew midgut volvulus.
Note the mesenteric attachment of the cecum. This
narrow stalk is more prone to volvulus. Additionally,
this stalk (Ladd's bands) is capable of compressing the
duodenum and obstructing it.
In a malrotation, many meters of intestine are free to
twist around this stalk, which, since it contains the
superior mesenteric artery, is vulnerable to
strangulation and ischemic necrosis. The occurrence of
this twisting and strangulation results in the surgical
emergency called midgut volvulus. Midgut volvulus
should not be confused with cecal or sigmoid volvulus.
Cecal and sigmoid volvulus generally occur in adults.
Sigmoid volvulus involves the large bowel and can often
be decompressed by barium enema or other
non-surgical procedures.
VIew midgut volvulus.
 In midgut volvulus, the majority of the small bowel is
involved in the stragulation. Substantial small bowel
necrosis occurs without prompt surgical intervention.
View cecal volvulus.
In midgut volvulus, the majority of the small bowel is
involved in the stragulation. Substantial small bowel
necrosis occurs without prompt surgical intervention.
View cecal volvulus.
 In malrotation, the cecum may be prone to twisting
or kinking if it is excessively mobile. Cecal volvulus can
occur in the absence of malrotation. This most often
presents in adults rather than children.
View sigmoid volvulus.
In malrotation, the cecum may be prone to twisting
or kinking if it is excessively mobile. Cecal volvulus can
occur in the absence of malrotation. This most often
presents in adults rather than children.
View sigmoid volvulus.
 Sigmoid volvulus is the most common site of colonic
volvulus. It occurs most often in the elderly. It is
associated with elongation of the descending colon
making the sigmoid region hypermobile and prone to
twisting.
Midgut volvulus is a surgical emergency at risk of
bowel infarction. Some neonatal examples of volvulus
are shown below.
View neonatal volvulus case.
Sigmoid volvulus is the most common site of colonic
volvulus. It occurs most often in the elderly. It is
associated with elongation of the descending colon
making the sigmoid region hypermobile and prone to
twisting.
Midgut volvulus is a surgical emergency at risk of
bowel infarction. Some neonatal examples of volvulus
are shown below.
View neonatal volvulus case.
 This radiograph of a 5-day old infant with vomiting
shows a gasless abdomen except for the small air
bubble in the stomach. Such a radiograph should be
considered highly suspicious for any type of upper GI
obstruction. Further studies on this infant showed a
midgut volvulus and malrotation.
View second neonatal case.
This radiograph of a 5-day old infant with vomiting
shows a gasless abdomen except for the small air
bubble in the stomach. Such a radiograph should be
considered highly suspicious for any type of upper GI
obstruction. Further studies on this infant showed a
midgut volvulus and malrotation.
View second neonatal case.
 This radiograph of a 9-day old infant with vomiting
looks relatively normal. It has a normal gas distribution
with no air fluid levels or excessively dilated loops.
Although this radiograph looks much more normal than
the first neonatal radiograph, further studies on this
infant also showed a midgut volvulus and malrotation.
Thus, it is not possible to rule out a volvulus due to
malrotation solely on plain films in some instances.
Clinical suspicion should lead one to pursue more
definitive radiographic studies. While sigmoid
volvulus usually shows severely dilated loops of bowel
and large air fluid levels on plain film radiographs, a
midgut volvulus may show non-specific findings on plain
films without the characteristic signs of an obvious
bowel obstruction.
View BE of second neonatal case.
This radiograph of a 9-day old infant with vomiting
looks relatively normal. It has a normal gas distribution
with no air fluid levels or excessively dilated loops.
Although this radiograph looks much more normal than
the first neonatal radiograph, further studies on this
infant also showed a midgut volvulus and malrotation.
Thus, it is not possible to rule out a volvulus due to
malrotation solely on plain films in some instances.
Clinical suspicion should lead one to pursue more
definitive radiographic studies. While sigmoid
volvulus usually shows severely dilated loops of bowel
and large air fluid levels on plain film radiographs, a
midgut volvulus may show non-specific findings on plain
films without the characteristic signs of an obvious
bowel obstruction.
View BE of second neonatal case.
 This is a barium enema of the infant above
which shows the ascending colon and cecum in the
wrong place. The cecum should normally be located in
the right lower quadrant, but in this BE, most of the
proximal large bowel is in the left upper quadrant. The
cecum is in the central abdomen.
In a patient who has a malrotation but is not
experiencing strangulation, malrotation is usually
identified on an upper GI series or barium enema. The
UGI series can more definitively determine the
presence of malrotation by identifying the position of the
ligament of Treitz. The BE can usually determine the
presence of malrotation by noting the malposition of the
cecum. It should normally be located in the right lower
quadrant. If the cecum is located elsewhere, then
malrotation is likely. However, both of these studies
can be deceiving at times. The ligament of Treitz may
be close to the normal location in a malrotation and the
cecum may occasionally be in the RLQ in a malrotation.
The classic presentation of malrotation is usually
described as a volvulus, heralded by bilious vomiting in
the first days of life. Less than half of the cases
actually present in the neonatal period. Catastrophic
midgut volvulus can present at any age. Lesser
degrees of reversible ischemia (sometimes called
intermittent volvulus), can produce intermittent pain,
non-bilious vomiting, gastroesophageal reflux,
malabsorption and failure to thrive. Patients with
malrotation may be entirely asymptomatic with
catastrophic volvulus occurring at any age. Neither the
age of the patient, nor the chronicity of symptoms are
predictive. All are at risk for severe complications (even
adults). The mortality of midgut volvulus in several
series is 40 to 60%. As some of these series date prior
to modern intensive care techniques, the current
mortality is probably lower, but the survivors may lose
so much bowel that they are totally dependent on
parenteral nutrition. Due to this significant mortality and
morbidity, even incidentally discovered malrotation
should be surgically corrected.
Intestinal obstruction is an uncommon cause of
vomiting in the pediatric age group. Most pediatric
vomiting is caused by infectious agents, including viral
gastroenteritis, but also associated with generalized
non-intestinal infections such as URI, otitis media and
pneumonia. Because of the relative preponderance of
benign causes of vomiting, the serious causes must
always be kept in mind and excluded or at least
anticipated in discharge instructions.
Vomiting in the neonatal period brings to mind
sepsis, congenital anomalies or meconium ileus. In the
first few months of life, pyloric stenosis, hernias and
intussusception are important causes of obstruction.
As the infant becomes mobile, foreign bodies and
poisoning must be considered. Abdominal trauma, both
intentional and accidental can produce vomiting.
In addition to the above, remember A-A-I-I-M-M
(AIM x2). The diagnosis of appendicitis is sometimes
obscure in the young patient. There are no reliable
tests to adequately exclude early appendicitis;
therefore, anticipation of the need for early
reexamination or observation in the emergency
department should be considered in any child with
abdominal pain and vomiting.
References
Powell DM, Othersen HB, Smith CD. Malrotation of
the Intestines in Children: The Effect of Age on
Presentation and Therapy. Journal of Pediatric Surgery
1989;24:777-780.
Andrassy RJ, Mahour GH. Malrotation of the Midgut
in Infants and Children, A 25 Year Review. Archives of
Surgery 1981;116:158-160.
Wang C, Welch CE. Anomalies of Intestinal
Rotation in Adolescents and Adults. Surgery
1963;54:839-855.
Ellenbourg DJ, Delcastillo J. Duodenal Obstruction
From Peritoneal (Ladd's) Bands in a Ten Year Old
Child. Annals of Emergency Medicine 1984;13:56-59.
Schnaufer L, Mahboubi S. Abdominal Emergencies.
In: Fleisher GR, Ludwig S (eds). Textbook of Pediatric
Emergency Medicine, third edition, 1993, Baltimore,
Williams and Wilkins, pp. 1307-1335.
Imbembo AL, Zucker KA. Volvulus of the colon. In:
Sabiston DC (ed). Textbook of Surgery, The Biological
Basis of Modern Surgical Practice, 14th edition.
Philadelphia, W.B. Saunders Company, 199, pp.
940-944.
Smith EI. Malrotation of the intestine. In: Welch
KJ, Randolph JG, Ravitch MM, O'Neill JA, Rowe MI
(eds). Pediatric Surgery, fourth edition. Chicago, Year
Book Medical Publishers, 1986, pp 882-895.
Malrotation. In: Raffensperger JG (ed). Swenson's
Pediatric Surgery, fifth edition. Norwalk, Connecticut,
Appleton & Lange, 1990, pp. 517-522.
This is a barium enema of the infant above
which shows the ascending colon and cecum in the
wrong place. The cecum should normally be located in
the right lower quadrant, but in this BE, most of the
proximal large bowel is in the left upper quadrant. The
cecum is in the central abdomen.
In a patient who has a malrotation but is not
experiencing strangulation, malrotation is usually
identified on an upper GI series or barium enema. The
UGI series can more definitively determine the
presence of malrotation by identifying the position of the
ligament of Treitz. The BE can usually determine the
presence of malrotation by noting the malposition of the
cecum. It should normally be located in the right lower
quadrant. If the cecum is located elsewhere, then
malrotation is likely. However, both of these studies
can be deceiving at times. The ligament of Treitz may
be close to the normal location in a malrotation and the
cecum may occasionally be in the RLQ in a malrotation.
The classic presentation of malrotation is usually
described as a volvulus, heralded by bilious vomiting in
the first days of life. Less than half of the cases
actually present in the neonatal period. Catastrophic
midgut volvulus can present at any age. Lesser
degrees of reversible ischemia (sometimes called
intermittent volvulus), can produce intermittent pain,
non-bilious vomiting, gastroesophageal reflux,
malabsorption and failure to thrive. Patients with
malrotation may be entirely asymptomatic with
catastrophic volvulus occurring at any age. Neither the
age of the patient, nor the chronicity of symptoms are
predictive. All are at risk for severe complications (even
adults). The mortality of midgut volvulus in several
series is 40 to 60%. As some of these series date prior
to modern intensive care techniques, the current
mortality is probably lower, but the survivors may lose
so much bowel that they are totally dependent on
parenteral nutrition. Due to this significant mortality and
morbidity, even incidentally discovered malrotation
should be surgically corrected.
Intestinal obstruction is an uncommon cause of
vomiting in the pediatric age group. Most pediatric
vomiting is caused by infectious agents, including viral
gastroenteritis, but also associated with generalized
non-intestinal infections such as URI, otitis media and
pneumonia. Because of the relative preponderance of
benign causes of vomiting, the serious causes must
always be kept in mind and excluded or at least
anticipated in discharge instructions.
Vomiting in the neonatal period brings to mind
sepsis, congenital anomalies or meconium ileus. In the
first few months of life, pyloric stenosis, hernias and
intussusception are important causes of obstruction.
As the infant becomes mobile, foreign bodies and
poisoning must be considered. Abdominal trauma, both
intentional and accidental can produce vomiting.
In addition to the above, remember A-A-I-I-M-M
(AIM x2). The diagnosis of appendicitis is sometimes
obscure in the young patient. There are no reliable
tests to adequately exclude early appendicitis;
therefore, anticipation of the need for early
reexamination or observation in the emergency
department should be considered in any child with
abdominal pain and vomiting.
References
Powell DM, Othersen HB, Smith CD. Malrotation of
the Intestines in Children: The Effect of Age on
Presentation and Therapy. Journal of Pediatric Surgery
1989;24:777-780.
Andrassy RJ, Mahour GH. Malrotation of the Midgut
in Infants and Children, A 25 Year Review. Archives of
Surgery 1981;116:158-160.
Wang C, Welch CE. Anomalies of Intestinal
Rotation in Adolescents and Adults. Surgery
1963;54:839-855.
Ellenbourg DJ, Delcastillo J. Duodenal Obstruction
From Peritoneal (Ladd's) Bands in a Ten Year Old
Child. Annals of Emergency Medicine 1984;13:56-59.
Schnaufer L, Mahboubi S. Abdominal Emergencies.
In: Fleisher GR, Ludwig S (eds). Textbook of Pediatric
Emergency Medicine, third edition, 1993, Baltimore,
Williams and Wilkins, pp. 1307-1335.
Imbembo AL, Zucker KA. Volvulus of the colon. In:
Sabiston DC (ed). Textbook of Surgery, The Biological
Basis of Modern Surgical Practice, 14th edition.
Philadelphia, W.B. Saunders Company, 199, pp.
940-944.
Smith EI. Malrotation of the intestine. In: Welch
KJ, Randolph JG, Ravitch MM, O'Neill JA, Rowe MI
(eds). Pediatric Surgery, fourth edition. Chicago, Year
Book Medical Publishers, 1986, pp 882-895.
Malrotation. In: Raffensperger JG (ed). Swenson's
Pediatric Surgery, fifth edition. Norwalk, Connecticut,
Appleton & Lange, 1990, pp. 517-522.