Moyamoya Disease
Radiology Cases in Pediatric Emergency Medicine
Volume 3, Case 9
Karen R. Sevigny Brown, MD
Loren G. Yamamoto, MD, MPH
Kapiolani Medical Center For Women And Children
University of Hawaii John A. Burns School of Medicine
This is a previously healthy, right-handed 7-year old
Asian female who presents to the E.D three hours after
developing right sided weakness of sudden onset. She
had been feeling well until noon, when she developed
weakness of her right hand and was unable to feed
herself. She sat up and tried to walk to her room. Her
father noted that her right leg was "crooked" and she
kept falling to the right. Her arm was "hanging to the
side" and was not swinging properly. Her father also
noted that her smile was "crooked." She has remained
alert through this illness. There is no history of fever,
trauma, seizures, loss of consciousness, headaches,
migraines or palpitations.
Exam: VS T37, P110, R24, BP 105/58. Weight 19
kg (10th percentile), Height 114 cm (10th percentile).
She is healthy appearing, cooperative, and alert in no
distress. She speaks well without dysarthria or
aphasia. Head normocephalic. Optic disc margins
sharp. TM's normal. Oral mucosa clear. Neck supple,
no bruits. Heart regular, grade 1/6 systolic ejection
murmur, vibratory in quality, at the left sternal border.
Lungs clear. Abdomen benign. Color and perfusion
are good.
Cranial nerve findings: Vision is intact. Pupils equal
and reactive. EOM's full. Peripheral fields full. Hearing
intact. Her tongue is midline. Her uvula deviates to the
left. There is an obvious flattening of the right
nasolabial fold and weakness of the right face.
Specifically, weak closure of the right eye and
movement of the forehead on the right. Her facial
sensation is intact. Her masseter function is not weak.
Trapezius function is good bilaterally.
Extremities: Using 4/4 as full strength, her right UE
is 2/4 and her right LE is 2/4. Her left side is not weak.
DTR's are 3+ bilaterally. There is a positive Babinski
sign on the right. Her left plantar reflex is downgoing.
Sensation is fully intact. Her observed gait is obviously
unsteady. She falls to the right. Her cerebellar function
is hard to test on her right because of her weakness.
Her left side is normal.
A CT scan is obtained. Before we see the result of
the CT scan, can you estimate where her CNS "lesion"
is likely to be.
1) Brain versus spinal cord ?
2) Are her findings due to a small lesion or a large
infarct as seen in the typical ACA (anterior cerebral
artery) and MCA (middle cerebral artery) distributions?
3) Is this likely to be a neoplasm, a hemorrhage, or
an infarct?
This is not a spinal cord lesion since she has
extensive facial involvement.
A large infarct is not likely since she is alert.
Additionally, her motor findings extend from her face to
her lower extremities without affecting speech and
language. This is most likely a smaller lesion.
The sudden onset makes a neoplasm less likely
although neoplasms can hemorrhage and undergo
sudden expansion. A hemorrhage is less likely since
her symptoms are not progressing, she has no
headache, and has no signs of increased intracranial
pressure. An infarct is uncommon in this age group,
however, a small infarct would account for her findings
and the sudden onset.
4) Where is her lesion likely to be?
It is most likely to be in a small area where the motor
fibers (both corticospinal and corticobulbar), originating
from the left brain, come together. Since her sensation
is unaffected, sensory pathways should be unaffected.
A likely possibility is the posterior limb of internal
capsule.
For a brief of review of the neuroanatomy of the
brain in this region, refer to the diagram at any time.
View neuroanatomy.
 L = Lateral ventricles. The anterior horns and the
posterior horns are shown in this diagram.
3 = Third ventricle.
CC = Corpus callosum.
C = Caudate nucleus.
P = Putamen
G = Globus Pallidus. The putamen and globus
pallidus together form the lenticular (lentiform) nucleus.
T = Thalamus
Arrows = Internal Capsule [anterior limb, posterior
limb, genu (bend)].
O = Optic radiations.
A = Auditory radiations.
The corticospinal tract originates from the motor
strip of the cerebral cortex. The fibers collect as they
traverse through the posterior limb of internal capsule.
The tract largely crosses the midline in the decussation
of the pyramids. Fibers exit the spinal cord at their
respective levels.
View our patient's CT scan.
L = Lateral ventricles. The anterior horns and the
posterior horns are shown in this diagram.
3 = Third ventricle.
CC = Corpus callosum.
C = Caudate nucleus.
P = Putamen
G = Globus Pallidus. The putamen and globus
pallidus together form the lenticular (lentiform) nucleus.
T = Thalamus
Arrows = Internal Capsule [anterior limb, posterior
limb, genu (bend)].
O = Optic radiations.
A = Auditory radiations.
The corticospinal tract originates from the motor
strip of the cerebral cortex. The fibers collect as they
traverse through the posterior limb of internal capsule.
The tract largely crosses the midline in the decussation
of the pyramids. Fibers exit the spinal cord at their
respective levels.
View our patient's CT scan.
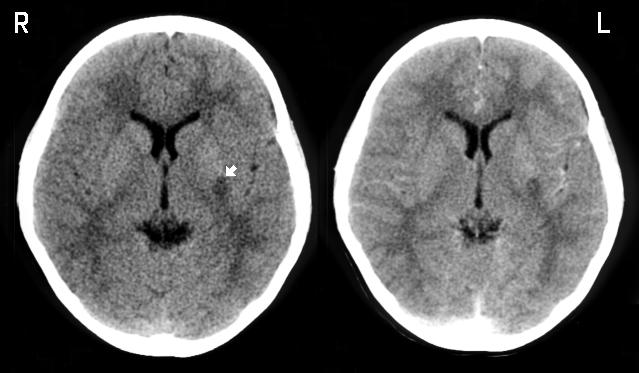
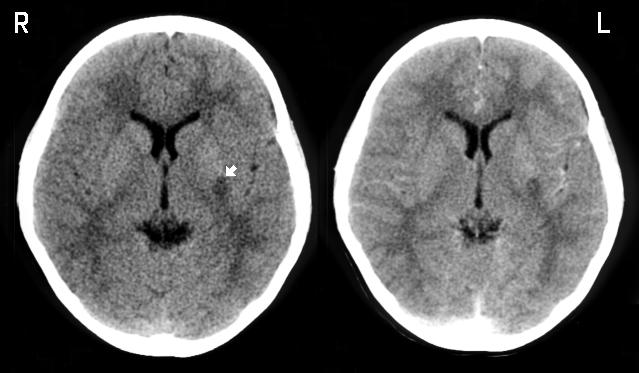 The image on the left is without contrast. The same
cut is shown on the right with contrast. The patient's
right is to the left of the image as marked. There is a
hypodense region in the left posterior basal ganglia.
The white arrow points to this region which is in the
area of the putamen adjacent to the posterior limb of
internal capsule. Although the neuroanatomy on the CT
scan is not well defined, you should still be able to
identify the caudate nucleus, the lenticular nucleus, and
the thalamus. The internal capsule can be identified
faintly. The posterior limb is located between the
thalamus and the lenticular nucleus. The anterior limb
is located between the caudate nucleus and the
lenticular nucleus. There is no significant mass
effect. This hypodensity does not enhance with
contrast suggesting that this is an ischemic lesion.
A pediatric neurologist is consulted and she is
admitted to the hospital. An MRI scan is obtained.
Magnetic resonance angiography (MRA) is also
performed.
View MRI scan.
The image on the left is without contrast. The same
cut is shown on the right with contrast. The patient's
right is to the left of the image as marked. There is a
hypodense region in the left posterior basal ganglia.
The white arrow points to this region which is in the
area of the putamen adjacent to the posterior limb of
internal capsule. Although the neuroanatomy on the CT
scan is not well defined, you should still be able to
identify the caudate nucleus, the lenticular nucleus, and
the thalamus. The internal capsule can be identified
faintly. The posterior limb is located between the
thalamus and the lenticular nucleus. The anterior limb
is located between the caudate nucleus and the
lenticular nucleus. There is no significant mass
effect. This hypodensity does not enhance with
contrast suggesting that this is an ischemic lesion.
A pediatric neurologist is consulted and she is
admitted to the hospital. An MRI scan is obtained.
Magnetic resonance angiography (MRA) is also
performed.
View MRI scan.
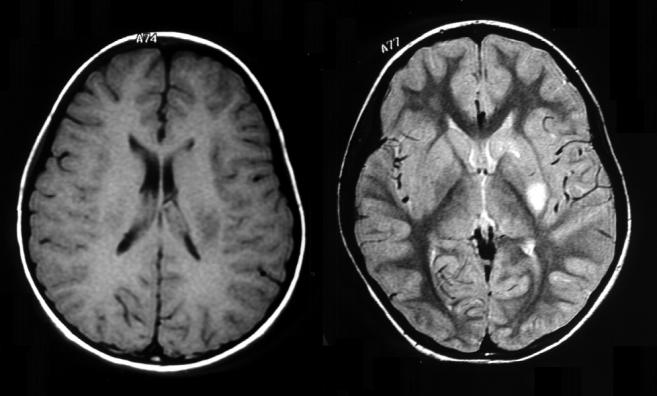
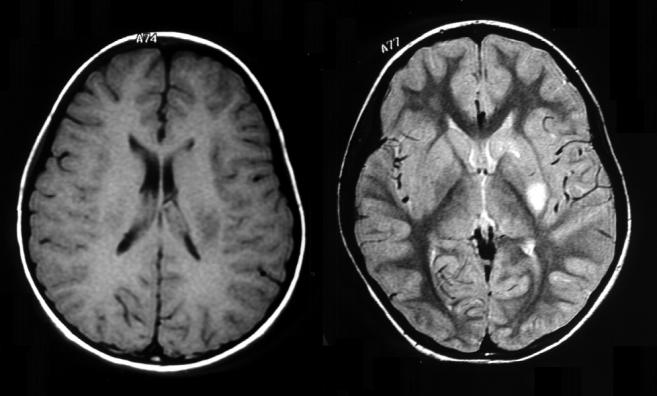 T1 (left image) and T2 (right image) weighted axial
images are shown (different levels). On the T1 image,
the ventricles appear to be dark and the infarct seen in
the left lenticular nucleus is dark as well. The T2 image
is a lower cut through the center of the infarct. The T2
image shows the CSF within the ventricles to be white.
The infarct appears as a white lesion in the caudate
nucleus and the left putamen. In the T2 image, internal
capsule is dark. Note the obvious distortion of the
anterior limb of the left internal capsule, compared to
the right. The posterior limb of the left internal capsule
is also slightly distorted (compared to the right) adjacent
to the infarct in the putamen. This study is read as an
infarct in the left basal ganglia, the posterior limb of
internal capsule, and the head of the caudate.
The structures of this T2 image are labeled if you
have difficulty identifying the structures.
T1 (left image) and T2 (right image) weighted axial
images are shown (different levels). On the T1 image,
the ventricles appear to be dark and the infarct seen in
the left lenticular nucleus is dark as well. The T2 image
is a lower cut through the center of the infarct. The T2
image shows the CSF within the ventricles to be white.
The infarct appears as a white lesion in the caudate
nucleus and the left putamen. In the T2 image, internal
capsule is dark. Note the obvious distortion of the
anterior limb of the left internal capsule, compared to
the right. The posterior limb of the left internal capsule
is also slightly distorted (compared to the right) adjacent
to the infarct in the putamen. This study is read as an
infarct in the left basal ganglia, the posterior limb of
internal capsule, and the head of the caudate.
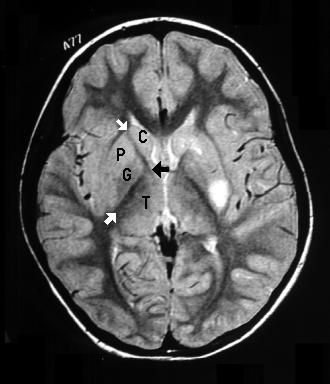
The structures of this T2 image are labeled if you
have difficulty identifying the structures.
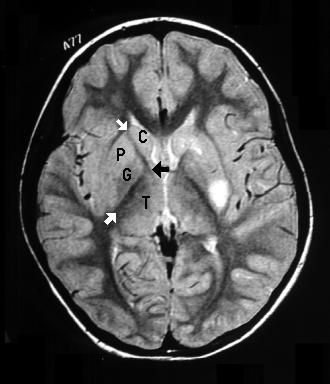 The white arrows point to the anterior and posterior limb
of internal capsule. The black arrow points to the genu.
The other labeled structures are the caudate nucleus
(C), globus pallidus (G), putamen (P), and thalamus
(T). The lateral ventricles are white.
View MRA study.
The white arrows point to the anterior and posterior limb
of internal capsule. The black arrow points to the genu.
The other labeled structures are the caudate nucleus
(C), globus pallidus (G), putamen (P), and thalamus
(T). The lateral ventricles are white.
View MRA study.
 There is obvious narrowing and irregularity of the left
internal carotid artery and its branches. The arrow on
the right points to the supraclinoid portion of the internal
carotid. The arrow on the left points to the horizonal
section of the anterior cerebral artery. She is
tentatively diagnosed with Moyamoya syndrome. An
angiogram is ordered.
View angiogram.
There is obvious narrowing and irregularity of the left
internal carotid artery and its branches. The arrow on
the right points to the supraclinoid portion of the internal
carotid. The arrow on the left points to the horizonal
section of the anterior cerebral artery. She is
tentatively diagnosed with Moyamoya syndrome. An
angiogram is ordered.
View angiogram.
 The image displayed here is an AP view of her left
internal carotid angiogram. The arrows point to
narrowed regions in the internal carotid artery and its
branches. The classic "puff of smoke" pattern seen in
Moyamoya disease was not visualized. This patient
turns out to have probable fibromuscular displasia (a
rare cerebrovascular disease).
View "puff of smoke".
The image displayed here is an AP view of her left
internal carotid angiogram. The arrows point to
narrowed regions in the internal carotid artery and its
branches. The classic "puff of smoke" pattern seen in
Moyamoya disease was not visualized. This patient
turns out to have probable fibromuscular displasia (a
rare cerebrovascular disease).
View "puff of smoke".
 The image displayed here is an internal carotid
angiogram taken from a different patient with a more
typical Moyamoya disease angiogram. The black arrow
points to the "puff of smoke" which represents
neovascularization providing collateral blood flow.
There is stenosis of the internal carotid artery proximal
to this puff of smoke. The white arrow points to a
dilated ophthalmic artery which is providing collateral
circulation as well.
Moyamoya disease is a disease of the large cerebral
vessels that results in a network of small collateral
vessels that form a pattern on angiography resembling
a "puff" or "hazy cloud" of smoke (the English
translation of the Japanese term, moyamoya).
Diseased vessels may narrow and occlude resulting in
transient ischemic attacks and/or cerebral infarcts, or
they may rupture resulting in spontaneous intracranial
hemorrhage. Patients may also present with
headaches. This condition presents largely in childhood
and is uncommon (Despite this, three likely cases have
been diagnosed in our center this year). Moyamoya is
often divided into a syndrome and a disease, however,
both are not specific. Not much is known about its
etiology. Its course typically results in progressive
neurological deterioration. While steroids and
vasodilators have little or no effect in the long term
outcome, a surgical procedure shunting intracerebral
vessels may have long term benefit. This patient's
angiographic studies are not diagnostic of Moyamoya.
This may be an early case of Moyamoya or some other
type of vasculopathy.
Strokes in Children
Stroke can be defined as an acute onset neurologic
deficit lasting more than one hour. The
pathophysiologic mechanisms for vascular dysfunction
include cerebral embolism, arterial and/or venous
thrombosis, and intraparenchymal/subarachnoid
hemorrhage. In contrast to adults, cerebral vascular
disease is not usually associated with atherosclerosis,
hypertension, or diabetes.
Sudden loss of function is usually characteristic for a
cerebral embolism. Incomplete improvement may be
seen as the embolus fragments and reperfusion occurs.
Cerebral embolism in children is most often associated
with cardiac disease.
Thrombotic infarction may be difficult to distinguish
from embolic infarction. Cerebral artery thrombosis
takes longer to develop than embolism and may be
preceded by transient ischemic attacks. In children,
arterial thrombosis is related to vasculopathy of cerebral
blood vessels, hemoglobinopathy, and vasculitis.
Venous thrombosis often presents with seizures and
increased intracranial pressure with the most common
causes including infection, dehydration,
hemoglobinopathy, and malignancy.
The presenting signs and symptoms of
intraparenchymal and subarachnoid hemorrhage
include severe headache, vomiting, and deterioration of
function. However, the findings may be very subtle,
such as alteration in mental status and a bulging
fontanelle in infants. Trauma, hematologic disorders
(sickle cell disease), vascular malformations (aneurysm
and arteriovenous malformations) and inflammatory
disease are among the most common causes of
strokes in children. Child abuse should be suspected in
any child with an unexplained intracranial hemorrhage.
When considering stroke in children, a diverse
differential diagnosis must be considered. Hemiplegia
with other focal deficits can follow a seizure (Todd's
paralysis). Usually this dysfunction resolves within 6
hours with complete resolution by 24 hours. A child
may frequently be found hemiplegic in the morning
following an unwitnessed nocturnal seizure. An
intracranial mass, either neoplasm or abscess, may
mimic a vascular lesion. Tumors may often
hemorrhage into a necrotic area, with localized
compression or invasion of intracranial vascular
structures. Infection must be considered since multiple
micro-infarcts are a common complication of bacterial
meningitis. Complicated and basilar migraines may be
accompanied by neurologic symptoms, with alternating
hemiplegia attributed to basilar migraine in children.
Several conditions cause stroke in children. Heart
disease is the most common of these, responsible for
one-third of all ischemic infarctions in children. Right to
left (cyanotic) intracardiac shunts can cause
polycythemia, leading to thrombosis and embolism.
Congenital heart disease with valvular defects and/or
cardiomyopathies can lead to thrombus formation and
stroke. Another common cause is hematologic
disorders such as sickle cell disease which is
associated with multiple infarcts. Coagulation disorders
such as hemophilia and platelet disorders have an
increased risk of intracranial hemorrhage and stroke.
Homocystinuria, an uncommon autosomal recessive
disorder, leads to an increased tendency for thrombosis
as a result of endothelial damage from excessive
homocystine, thus leading to platelet aggregation and
thrombus formation. Inherited disorders of the blood
vessel wall can result in hemorrhage (AVM's,
aneurysms, tuberous sclerosis, neurofibromatosis,
hereditary hemorrhagic telangiectasia, fibromuscular
dysplasia, von Hippel-Lindau syndrome, and Fabry
disease).
References
Riela AR, Roach ES. Etiology of Stoke in Children.
Journal of Child Neurology 1993;8:201-220.
Pavlakis SG, Gould RJ, Zito JL. Stroke in Children.
Advances in Pediatrics 1991:151-179.
Matsushima Y, Aoyagi M, Niimi Y, Masaoka H,
Ohno K. Symptoms and Their Pattern of Progression
in Childhood Moyamoya Disease. Brain &
Development 1990;12:784.
Rooney CM, Kaye EM, Scott M, Klucznik RP,
Rosman NP. Modified Encephaloduro-
arteriosynangiosis as a Surgical Treatment of
Childhood Moyamoya Disease: Report of Five Cases.
Journal of Child Neurology 1991;6:24-31.
The image displayed here is an internal carotid
angiogram taken from a different patient with a more
typical Moyamoya disease angiogram. The black arrow
points to the "puff of smoke" which represents
neovascularization providing collateral blood flow.
There is stenosis of the internal carotid artery proximal
to this puff of smoke. The white arrow points to a
dilated ophthalmic artery which is providing collateral
circulation as well.
Moyamoya disease is a disease of the large cerebral
vessels that results in a network of small collateral
vessels that form a pattern on angiography resembling
a "puff" or "hazy cloud" of smoke (the English
translation of the Japanese term, moyamoya).
Diseased vessels may narrow and occlude resulting in
transient ischemic attacks and/or cerebral infarcts, or
they may rupture resulting in spontaneous intracranial
hemorrhage. Patients may also present with
headaches. This condition presents largely in childhood
and is uncommon (Despite this, three likely cases have
been diagnosed in our center this year). Moyamoya is
often divided into a syndrome and a disease, however,
both are not specific. Not much is known about its
etiology. Its course typically results in progressive
neurological deterioration. While steroids and
vasodilators have little or no effect in the long term
outcome, a surgical procedure shunting intracerebral
vessels may have long term benefit. This patient's
angiographic studies are not diagnostic of Moyamoya.
This may be an early case of Moyamoya or some other
type of vasculopathy.
Strokes in Children
Stroke can be defined as an acute onset neurologic
deficit lasting more than one hour. The
pathophysiologic mechanisms for vascular dysfunction
include cerebral embolism, arterial and/or venous
thrombosis, and intraparenchymal/subarachnoid
hemorrhage. In contrast to adults, cerebral vascular
disease is not usually associated with atherosclerosis,
hypertension, or diabetes.
Sudden loss of function is usually characteristic for a
cerebral embolism. Incomplete improvement may be
seen as the embolus fragments and reperfusion occurs.
Cerebral embolism in children is most often associated
with cardiac disease.
Thrombotic infarction may be difficult to distinguish
from embolic infarction. Cerebral artery thrombosis
takes longer to develop than embolism and may be
preceded by transient ischemic attacks. In children,
arterial thrombosis is related to vasculopathy of cerebral
blood vessels, hemoglobinopathy, and vasculitis.
Venous thrombosis often presents with seizures and
increased intracranial pressure with the most common
causes including infection, dehydration,
hemoglobinopathy, and malignancy.
The presenting signs and symptoms of
intraparenchymal and subarachnoid hemorrhage
include severe headache, vomiting, and deterioration of
function. However, the findings may be very subtle,
such as alteration in mental status and a bulging
fontanelle in infants. Trauma, hematologic disorders
(sickle cell disease), vascular malformations (aneurysm
and arteriovenous malformations) and inflammatory
disease are among the most common causes of
strokes in children. Child abuse should be suspected in
any child with an unexplained intracranial hemorrhage.
When considering stroke in children, a diverse
differential diagnosis must be considered. Hemiplegia
with other focal deficits can follow a seizure (Todd's
paralysis). Usually this dysfunction resolves within 6
hours with complete resolution by 24 hours. A child
may frequently be found hemiplegic in the morning
following an unwitnessed nocturnal seizure. An
intracranial mass, either neoplasm or abscess, may
mimic a vascular lesion. Tumors may often
hemorrhage into a necrotic area, with localized
compression or invasion of intracranial vascular
structures. Infection must be considered since multiple
micro-infarcts are a common complication of bacterial
meningitis. Complicated and basilar migraines may be
accompanied by neurologic symptoms, with alternating
hemiplegia attributed to basilar migraine in children.
Several conditions cause stroke in children. Heart
disease is the most common of these, responsible for
one-third of all ischemic infarctions in children. Right to
left (cyanotic) intracardiac shunts can cause
polycythemia, leading to thrombosis and embolism.
Congenital heart disease with valvular defects and/or
cardiomyopathies can lead to thrombus formation and
stroke. Another common cause is hematologic
disorders such as sickle cell disease which is
associated with multiple infarcts. Coagulation disorders
such as hemophilia and platelet disorders have an
increased risk of intracranial hemorrhage and stroke.
Homocystinuria, an uncommon autosomal recessive
disorder, leads to an increased tendency for thrombosis
as a result of endothelial damage from excessive
homocystine, thus leading to platelet aggregation and
thrombus formation. Inherited disorders of the blood
vessel wall can result in hemorrhage (AVM's,
aneurysms, tuberous sclerosis, neurofibromatosis,
hereditary hemorrhagic telangiectasia, fibromuscular
dysplasia, von Hippel-Lindau syndrome, and Fabry
disease).
References
Riela AR, Roach ES. Etiology of Stoke in Children.
Journal of Child Neurology 1993;8:201-220.
Pavlakis SG, Gould RJ, Zito JL. Stroke in Children.
Advances in Pediatrics 1991:151-179.
Matsushima Y, Aoyagi M, Niimi Y, Masaoka H,
Ohno K. Symptoms and Their Pattern of Progression
in Childhood Moyamoya Disease. Brain &
Development 1990;12:784.
Rooney CM, Kaye EM, Scott M, Klucznik RP,
Rosman NP. Modified Encephaloduro-
arteriosynangiosis as a Surgical Treatment of
Childhood Moyamoya Disease: Report of Five Cases.
Journal of Child Neurology 1991;6:24-31.
Return to Radiology Cases In Ped Emerg Med Case Selection Page
Return to Univ. Hawaii Dept. Pediatrics Home Page
 L = Lateral ventricles. The anterior horns and the
posterior horns are shown in this diagram.
3 = Third ventricle.
CC = Corpus callosum.
C = Caudate nucleus.
P = Putamen
G = Globus Pallidus. The putamen and globus
pallidus together form the lenticular (lentiform) nucleus.
T = Thalamus
Arrows = Internal Capsule [anterior limb, posterior
limb, genu (bend)].
O = Optic radiations.
A = Auditory radiations.
The corticospinal tract originates from the motor
strip of the cerebral cortex. The fibers collect as they
traverse through the posterior limb of internal capsule.
The tract largely crosses the midline in the decussation
of the pyramids. Fibers exit the spinal cord at their
respective levels.
View our patient's CT scan.
L = Lateral ventricles. The anterior horns and the
posterior horns are shown in this diagram.
3 = Third ventricle.
CC = Corpus callosum.
C = Caudate nucleus.
P = Putamen
G = Globus Pallidus. The putamen and globus
pallidus together form the lenticular (lentiform) nucleus.
T = Thalamus
Arrows = Internal Capsule [anterior limb, posterior
limb, genu (bend)].
O = Optic radiations.
A = Auditory radiations.
The corticospinal tract originates from the motor
strip of the cerebral cortex. The fibers collect as they
traverse through the posterior limb of internal capsule.
The tract largely crosses the midline in the decussation
of the pyramids. Fibers exit the spinal cord at their
respective levels.
View our patient's CT scan.
 The image on the left is without contrast. The same
cut is shown on the right with contrast. The patient's
right is to the left of the image as marked. There is a
hypodense region in the left posterior basal ganglia.
The white arrow points to this region which is in the
area of the putamen adjacent to the posterior limb of
internal capsule. Although the neuroanatomy on the CT
scan is not well defined, you should still be able to
identify the caudate nucleus, the lenticular nucleus, and
the thalamus. The internal capsule can be identified
faintly. The posterior limb is located between the
thalamus and the lenticular nucleus. The anterior limb
is located between the caudate nucleus and the
lenticular nucleus. There is no significant mass
effect. This hypodensity does not enhance with
contrast suggesting that this is an ischemic lesion.
A pediatric neurologist is consulted and she is
admitted to the hospital. An MRI scan is obtained.
Magnetic resonance angiography (MRA) is also
performed.
View MRI scan.
The image on the left is without contrast. The same
cut is shown on the right with contrast. The patient's
right is to the left of the image as marked. There is a
hypodense region in the left posterior basal ganglia.
The white arrow points to this region which is in the
area of the putamen adjacent to the posterior limb of
internal capsule. Although the neuroanatomy on the CT
scan is not well defined, you should still be able to
identify the caudate nucleus, the lenticular nucleus, and
the thalamus. The internal capsule can be identified
faintly. The posterior limb is located between the
thalamus and the lenticular nucleus. The anterior limb
is located between the caudate nucleus and the
lenticular nucleus. There is no significant mass
effect. This hypodensity does not enhance with
contrast suggesting that this is an ischemic lesion.
A pediatric neurologist is consulted and she is
admitted to the hospital. An MRI scan is obtained.
Magnetic resonance angiography (MRA) is also
performed.
View MRI scan.
 T1 (left image) and T2 (right image) weighted axial
images are shown (different levels). On the T1 image,
the ventricles appear to be dark and the infarct seen in
the left lenticular nucleus is dark as well. The T2 image
is a lower cut through the center of the infarct. The T2
image shows the CSF within the ventricles to be white.
The infarct appears as a white lesion in the caudate
nucleus and the left putamen. In the T2 image, internal
capsule is dark. Note the obvious distortion of the
anterior limb of the left internal capsule, compared to
the right. The posterior limb of the left internal capsule
is also slightly distorted (compared to the right) adjacent
to the infarct in the putamen. This study is read as an
infarct in the left basal ganglia, the posterior limb of
internal capsule, and the head of the caudate.
The structures of this T2 image are labeled if you
have difficulty identifying the structures.
T1 (left image) and T2 (right image) weighted axial
images are shown (different levels). On the T1 image,
the ventricles appear to be dark and the infarct seen in
the left lenticular nucleus is dark as well. The T2 image
is a lower cut through the center of the infarct. The T2
image shows the CSF within the ventricles to be white.
The infarct appears as a white lesion in the caudate
nucleus and the left putamen. In the T2 image, internal
capsule is dark. Note the obvious distortion of the
anterior limb of the left internal capsule, compared to
the right. The posterior limb of the left internal capsule
is also slightly distorted (compared to the right) adjacent
to the infarct in the putamen. This study is read as an
infarct in the left basal ganglia, the posterior limb of
internal capsule, and the head of the caudate.
The structures of this T2 image are labeled if you
have difficulty identifying the structures.
 The white arrows point to the anterior and posterior limb
of internal capsule. The black arrow points to the genu.
The other labeled structures are the caudate nucleus
(C), globus pallidus (G), putamen (P), and thalamus
(T). The lateral ventricles are white.
View MRA study.
The white arrows point to the anterior and posterior limb
of internal capsule. The black arrow points to the genu.
The other labeled structures are the caudate nucleus
(C), globus pallidus (G), putamen (P), and thalamus
(T). The lateral ventricles are white.
View MRA study.
 There is obvious narrowing and irregularity of the left
internal carotid artery and its branches. The arrow on
the right points to the supraclinoid portion of the internal
carotid. The arrow on the left points to the horizonal
section of the anterior cerebral artery. She is
tentatively diagnosed with Moyamoya syndrome. An
angiogram is ordered.
View angiogram.
There is obvious narrowing and irregularity of the left
internal carotid artery and its branches. The arrow on
the right points to the supraclinoid portion of the internal
carotid. The arrow on the left points to the horizonal
section of the anterior cerebral artery. She is
tentatively diagnosed with Moyamoya syndrome. An
angiogram is ordered.
View angiogram.
 The image displayed here is an AP view of her left
internal carotid angiogram. The arrows point to
narrowed regions in the internal carotid artery and its
branches. The classic "puff of smoke" pattern seen in
Moyamoya disease was not visualized. This patient
turns out to have probable fibromuscular displasia (a
rare cerebrovascular disease).
View "puff of smoke".
The image displayed here is an AP view of her left
internal carotid angiogram. The arrows point to
narrowed regions in the internal carotid artery and its
branches. The classic "puff of smoke" pattern seen in
Moyamoya disease was not visualized. This patient
turns out to have probable fibromuscular displasia (a
rare cerebrovascular disease).
View "puff of smoke".
 The image displayed here is an internal carotid
angiogram taken from a different patient with a more
typical Moyamoya disease angiogram. The black arrow
points to the "puff of smoke" which represents
neovascularization providing collateral blood flow.
There is stenosis of the internal carotid artery proximal
to this puff of smoke. The white arrow points to a
dilated ophthalmic artery which is providing collateral
circulation as well.
Moyamoya disease is a disease of the large cerebral
vessels that results in a network of small collateral
vessels that form a pattern on angiography resembling
a "puff" or "hazy cloud" of smoke (the English
translation of the Japanese term, moyamoya).
Diseased vessels may narrow and occlude resulting in
transient ischemic attacks and/or cerebral infarcts, or
they may rupture resulting in spontaneous intracranial
hemorrhage. Patients may also present with
headaches. This condition presents largely in childhood
and is uncommon (Despite this, three likely cases have
been diagnosed in our center this year). Moyamoya is
often divided into a syndrome and a disease, however,
both are not specific. Not much is known about its
etiology. Its course typically results in progressive
neurological deterioration. While steroids and
vasodilators have little or no effect in the long term
outcome, a surgical procedure shunting intracerebral
vessels may have long term benefit. This patient's
angiographic studies are not diagnostic of Moyamoya.
This may be an early case of Moyamoya or some other
type of vasculopathy.
Strokes in Children
Stroke can be defined as an acute onset neurologic
deficit lasting more than one hour. The
pathophysiologic mechanisms for vascular dysfunction
include cerebral embolism, arterial and/or venous
thrombosis, and intraparenchymal/subarachnoid
hemorrhage. In contrast to adults, cerebral vascular
disease is not usually associated with atherosclerosis,
hypertension, or diabetes.
Sudden loss of function is usually characteristic for a
cerebral embolism. Incomplete improvement may be
seen as the embolus fragments and reperfusion occurs.
Cerebral embolism in children is most often associated
with cardiac disease.
Thrombotic infarction may be difficult to distinguish
from embolic infarction. Cerebral artery thrombosis
takes longer to develop than embolism and may be
preceded by transient ischemic attacks. In children,
arterial thrombosis is related to vasculopathy of cerebral
blood vessels, hemoglobinopathy, and vasculitis.
Venous thrombosis often presents with seizures and
increased intracranial pressure with the most common
causes including infection, dehydration,
hemoglobinopathy, and malignancy.
The presenting signs and symptoms of
intraparenchymal and subarachnoid hemorrhage
include severe headache, vomiting, and deterioration of
function. However, the findings may be very subtle,
such as alteration in mental status and a bulging
fontanelle in infants. Trauma, hematologic disorders
(sickle cell disease), vascular malformations (aneurysm
and arteriovenous malformations) and inflammatory
disease are among the most common causes of
strokes in children. Child abuse should be suspected in
any child with an unexplained intracranial hemorrhage.
When considering stroke in children, a diverse
differential diagnosis must be considered. Hemiplegia
with other focal deficits can follow a seizure (Todd's
paralysis). Usually this dysfunction resolves within 6
hours with complete resolution by 24 hours. A child
may frequently be found hemiplegic in the morning
following an unwitnessed nocturnal seizure. An
intracranial mass, either neoplasm or abscess, may
mimic a vascular lesion. Tumors may often
hemorrhage into a necrotic area, with localized
compression or invasion of intracranial vascular
structures. Infection must be considered since multiple
micro-infarcts are a common complication of bacterial
meningitis. Complicated and basilar migraines may be
accompanied by neurologic symptoms, with alternating
hemiplegia attributed to basilar migraine in children.
Several conditions cause stroke in children. Heart
disease is the most common of these, responsible for
one-third of all ischemic infarctions in children. Right to
left (cyanotic) intracardiac shunts can cause
polycythemia, leading to thrombosis and embolism.
Congenital heart disease with valvular defects and/or
cardiomyopathies can lead to thrombus formation and
stroke. Another common cause is hematologic
disorders such as sickle cell disease which is
associated with multiple infarcts. Coagulation disorders
such as hemophilia and platelet disorders have an
increased risk of intracranial hemorrhage and stroke.
Homocystinuria, an uncommon autosomal recessive
disorder, leads to an increased tendency for thrombosis
as a result of endothelial damage from excessive
homocystine, thus leading to platelet aggregation and
thrombus formation. Inherited disorders of the blood
vessel wall can result in hemorrhage (AVM's,
aneurysms, tuberous sclerosis, neurofibromatosis,
hereditary hemorrhagic telangiectasia, fibromuscular
dysplasia, von Hippel-Lindau syndrome, and Fabry
disease).
References
Riela AR, Roach ES. Etiology of Stoke in Children.
Journal of Child Neurology 1993;8:201-220.
Pavlakis SG, Gould RJ, Zito JL. Stroke in Children.
Advances in Pediatrics 1991:151-179.
Matsushima Y, Aoyagi M, Niimi Y, Masaoka H,
Ohno K. Symptoms and Their Pattern of Progression
in Childhood Moyamoya Disease. Brain &
Development 1990;12:784.
Rooney CM, Kaye EM, Scott M, Klucznik RP,
Rosman NP. Modified Encephaloduro-
arteriosynangiosis as a Surgical Treatment of
Childhood Moyamoya Disease: Report of Five Cases.
Journal of Child Neurology 1991;6:24-31.
The image displayed here is an internal carotid
angiogram taken from a different patient with a more
typical Moyamoya disease angiogram. The black arrow
points to the "puff of smoke" which represents
neovascularization providing collateral blood flow.
There is stenosis of the internal carotid artery proximal
to this puff of smoke. The white arrow points to a
dilated ophthalmic artery which is providing collateral
circulation as well.
Moyamoya disease is a disease of the large cerebral
vessels that results in a network of small collateral
vessels that form a pattern on angiography resembling
a "puff" or "hazy cloud" of smoke (the English
translation of the Japanese term, moyamoya).
Diseased vessels may narrow and occlude resulting in
transient ischemic attacks and/or cerebral infarcts, or
they may rupture resulting in spontaneous intracranial
hemorrhage. Patients may also present with
headaches. This condition presents largely in childhood
and is uncommon (Despite this, three likely cases have
been diagnosed in our center this year). Moyamoya is
often divided into a syndrome and a disease, however,
both are not specific. Not much is known about its
etiology. Its course typically results in progressive
neurological deterioration. While steroids and
vasodilators have little or no effect in the long term
outcome, a surgical procedure shunting intracerebral
vessels may have long term benefit. This patient's
angiographic studies are not diagnostic of Moyamoya.
This may be an early case of Moyamoya or some other
type of vasculopathy.
Strokes in Children
Stroke can be defined as an acute onset neurologic
deficit lasting more than one hour. The
pathophysiologic mechanisms for vascular dysfunction
include cerebral embolism, arterial and/or venous
thrombosis, and intraparenchymal/subarachnoid
hemorrhage. In contrast to adults, cerebral vascular
disease is not usually associated with atherosclerosis,
hypertension, or diabetes.
Sudden loss of function is usually characteristic for a
cerebral embolism. Incomplete improvement may be
seen as the embolus fragments and reperfusion occurs.
Cerebral embolism in children is most often associated
with cardiac disease.
Thrombotic infarction may be difficult to distinguish
from embolic infarction. Cerebral artery thrombosis
takes longer to develop than embolism and may be
preceded by transient ischemic attacks. In children,
arterial thrombosis is related to vasculopathy of cerebral
blood vessels, hemoglobinopathy, and vasculitis.
Venous thrombosis often presents with seizures and
increased intracranial pressure with the most common
causes including infection, dehydration,
hemoglobinopathy, and malignancy.
The presenting signs and symptoms of
intraparenchymal and subarachnoid hemorrhage
include severe headache, vomiting, and deterioration of
function. However, the findings may be very subtle,
such as alteration in mental status and a bulging
fontanelle in infants. Trauma, hematologic disorders
(sickle cell disease), vascular malformations (aneurysm
and arteriovenous malformations) and inflammatory
disease are among the most common causes of
strokes in children. Child abuse should be suspected in
any child with an unexplained intracranial hemorrhage.
When considering stroke in children, a diverse
differential diagnosis must be considered. Hemiplegia
with other focal deficits can follow a seizure (Todd's
paralysis). Usually this dysfunction resolves within 6
hours with complete resolution by 24 hours. A child
may frequently be found hemiplegic in the morning
following an unwitnessed nocturnal seizure. An
intracranial mass, either neoplasm or abscess, may
mimic a vascular lesion. Tumors may often
hemorrhage into a necrotic area, with localized
compression or invasion of intracranial vascular
structures. Infection must be considered since multiple
micro-infarcts are a common complication of bacterial
meningitis. Complicated and basilar migraines may be
accompanied by neurologic symptoms, with alternating
hemiplegia attributed to basilar migraine in children.
Several conditions cause stroke in children. Heart
disease is the most common of these, responsible for
one-third of all ischemic infarctions in children. Right to
left (cyanotic) intracardiac shunts can cause
polycythemia, leading to thrombosis and embolism.
Congenital heart disease with valvular defects and/or
cardiomyopathies can lead to thrombus formation and
stroke. Another common cause is hematologic
disorders such as sickle cell disease which is
associated with multiple infarcts. Coagulation disorders
such as hemophilia and platelet disorders have an
increased risk of intracranial hemorrhage and stroke.
Homocystinuria, an uncommon autosomal recessive
disorder, leads to an increased tendency for thrombosis
as a result of endothelial damage from excessive
homocystine, thus leading to platelet aggregation and
thrombus formation. Inherited disorders of the blood
vessel wall can result in hemorrhage (AVM's,
aneurysms, tuberous sclerosis, neurofibromatosis,
hereditary hemorrhagic telangiectasia, fibromuscular
dysplasia, von Hippel-Lindau syndrome, and Fabry
disease).
References
Riela AR, Roach ES. Etiology of Stoke in Children.
Journal of Child Neurology 1993;8:201-220.
Pavlakis SG, Gould RJ, Zito JL. Stroke in Children.
Advances in Pediatrics 1991:151-179.
Matsushima Y, Aoyagi M, Niimi Y, Masaoka H,
Ohno K. Symptoms and Their Pattern of Progression
in Childhood Moyamoya Disease. Brain &
Development 1990;12:784.
Rooney CM, Kaye EM, Scott M, Klucznik RP,
Rosman NP. Modified Encephaloduro-
arteriosynangiosis as a Surgical Treatment of
Childhood Moyamoya Disease: Report of Five Cases.
Journal of Child Neurology 1991;6:24-31.