Severe Hyponatremia and Non-Reactive Pupils in a 3-Year Old
Radiology Cases in Pediatric Emergency Medicine
Volume 3, Case 15
Loren G. Yamamoto, MD, MPH
Kapiolani Medical Center For Women And Children
University of Hawaii John A. Burns School of Medicine
To most effectively appreciate the findings in this
case, it is recommended that you review the previous
case (Case 14 in Volume 3, Severe Hypernatremia -
Salt Poisoning) prior to reviewing this case.
A 3-year old male who is a recent immigrant from
Asia is seen in a physician's office following a 4-minute
seizure. He appears to be lethargic. Without much of
an evaluation, his parents are told to drive him to the
hospital for admission. He is seen on the pediatric ward
by a first year resident who obtains the following
information.
He has been in the U.S. for one month and has not
seen a physician in the U.S. until today. He has been
having fevers up to 40 degrees for the past two days.
Today, he did not feel hot, but his parents describe a
4-minute generalized seizure. Over the past two days
his condition has worsened. He is weak and can no
longer get up or walk around. He has a mild cough,
occasional loose stools, and about three episodes of
emesis per day for the past two days. He has not been
eating well. His only fluid intake has been three cups of
rice soup per day. A friend told the family to spoon feed
him a small amount at a time and they have tried to do
this.
His past history is significant for "being a little slow".
Further questioning reveals that he can only say two
words (mother and father) in his native Asian language.
His birthweight was 3.5 kg. He was bottle fed, but to
date, he cannot feed himself. He must be fed by his
parents (even before this illness). He is fed soft table
foods. He underwent a language test in his birth
country which he did very poorly on. He underwent a
hearing test of some type which was reportedly normal.
His vision is also in question since at an earlier age, he
would bump into walls frequently. However, in the past
9 months, he has been doing this less often. One of his
physicians in his birth country felt that he was autistic.
Exam: VS T37.4 (rectal), P120, R25, BP 88/64.
Weight 15.5 kg (50th percentile), height 90th percentile.
He is lethargic and moaning. His body is well
developed and nourished. He has no dysmorphic
features. He is not toxic or irritable. There is no
respiratory distress evident. His visible perfusion and
color are good. Head normocephalic without external
signs of head trauma. Pupils 7mm and not reactive to
light. His eyes are roughly conjugate, but he does not
follow objects. His eyes do not blink with sudden
confrontation. Fundi show sharp disc margins.
However, the discs are extremely pale, practically
resembling a large pit. There is no cup within the disc.
The retina is very pale with a sparse paucity of blood
vessels. Those blood vessels that are present are very
thin. The normal vessels coming through the optic disc
are extremely thin. His fundi are easy to view since his
pupils are dilated and do not constrict.
His neck, heart, lungs, and abdomen are normal.
His facial function is good. He is generally hyporeflexic
and hypotonic. Babinski signs are positive bilaterally.
A CBC, chemistry panel, and a CT scan of the head
are ordered. A complex patient is currently on the CT
scanner and a delay of at least 2 hours is anticipated
before our patient can be scanned (this case actually
takes place in the early 1980's). The following lab
results return before the CT scan is performed:
Na 97, K 1.6, Cl 54, Bicarb 28
BUN 3.0, creat 0.6, glucose 110
Ammonia 7.0, SGOT 94
CBC WBC 9.1, 53% segs, 44% lymphs, Hgb 10.9,
Hct 33.9, platelets 300,000.
The first year resident contacts the senior resident
and informs the senior resident that this patient has a
sodium of 97 with non-reactive pupils. The first year
resident is told that these findings are not compatible
with life. The senior resident arrives and concurs that
the pupils are dilated and non-reactive. He draws
another blood sample via a radial artery puncture:
ABG in room air: pH 7.57, pCO2 30, pO2 80, BE +6
Na 97 with the other electrolytes essentially the same.
In evaluating a patient with hyponatremia, a urine
sodium measurement is very useful in narrowing the
differential diagnosis. However, the urine sodium must
be obtained while the patient is hyponatremic for it to be
useful. Once the patient is normonatremic, the urine
sodium value can be anything. In hyponatremic
patients, their urine sodium should be low (less than 10
mEq/liter). A high value indicates that the kidneys are
inappropriately wasting sodium. Examples of such
conditions include SIADH (syndrome of inappropriate
antidiuretic hormone), mineralocorticoid deficiency (eg.,
Addisonian crisis), diuretics (eg., furosemide, thiazides,
etc.), and a salt losing nephropathy (in a patient with
renal disease). In the rush to correct our patient's
hyponatremia, a urine sodium was ordered, however, it
was not actually collected until the patient was already
receiving sodium supplements.
There was some question as to whether this child
was chronically water intoxicated as a result of child
abuse. His non-reactive pupils and developmental
delays could possibly represent a severe CNS injury
sustained any time in the past.
Water intoxication has been described as a
syndrome of child abuse if water is forcibly administered
to a child, usually as punishment. Once water is forced
in the mouth, if the child is too young to spit it out, it
must be swallowed. Case reports of forced water
intoxication describe children who were forced to drink
many glasses of water. Another case described the
parents forcing a water hose in the child's mouth.
Another case described a child with severe
hyponatremia due to water administration and water
enemas. The water is often used as a punishment for
bed wetting. These cases are often associated with
other signs of child abuse such as fractures, bruises,
burns, or failure to thrive. However, in the cases
described in the literature, these children had sodium
values in the 108 to 122 mEq/liter range.
After reviewing the previous case, Case 15 (Severe
Hypernatremia - Salt Poisoning), the factors
surrounding forcible salt poisoning and forcible water
intoxication are very similar with respect to child abuse,
however, the opposite extremes of sodium result.
Causes of hyponatremia not associated with
deliberate child abuse include infant swimming lessons
(infants swallow a lot of water while "swimming"),
excessive dilution of infant formula, and drinking large
amounts of cold water to help with a toothache.
Teenagers and adults have been known to drink large
amounts of water prior to urine drug testing to dilute
their urine as much as possible to minimize the chance
of drug detection.
Further history from our patient's family did not
suggest child abuse. In addition to the child's mother,
four siblings of the child were present. None of them
noted that the child was fed an excessive amount of
water.
Questions:
Can you explain his clinical findings ?
In summary, his findings consist of fever, a seizure,
hyponatremia, hypokalemia, non-reactive pupils,
blindness, optic atrophy, and developmental delays.
However, he was able to walk around prior to his
current illness.
The CT scan is completed.
View CT scan.
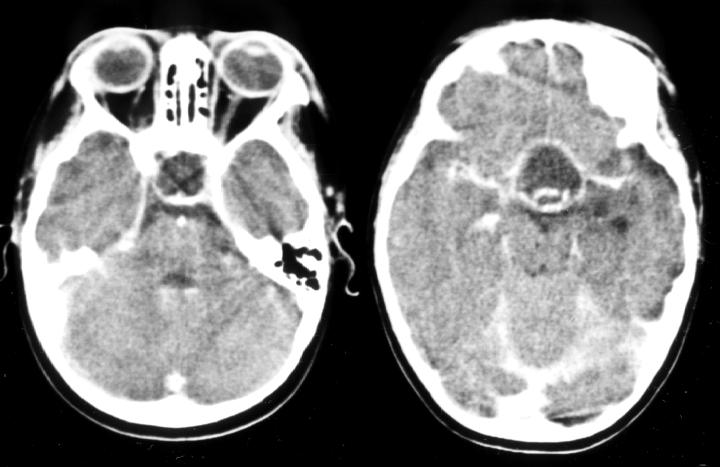 This CT scan shows a 2.5cm cystic partially calcified
suprasellar mass which undergoes peripheral
enhancement with contrast. This is most likely a
craniopharyngioma. Other structures such as the
tentorium are also enhancing.
His non-reactive pupils are due to erosion of the
optic nerves. His fundoscopic findings are due to
severe optic atrophy. It is difficult to believe that the
child's family could not tell that he was blind. His motor
and developmental delays are now well explained. It is
amazing that this child could walk around. It is not
surprising that he would bump into the walls since he
could not see.
His severe hyponatremia is probably longstanding.
Only a child with chronic hyponatremia would be able to
tolerate such a low sodium value of 97 mEq/liter.
Although this patient probably had long standing
panhypopituitarism it is unclear why both his growth
and his glucose homeostasis were satisfactory.
One would expect that he should have growth hormone
deficiency and insufficient adrenal stimulation.
Diabetes insipidus would not account for his
hyponatremia since diabetes insipidus should result in
hypernatremia. Hypoaldosteronism coupled with
SIADH could explain this, but this degree of
hyponatremia is so severe that a concomitant element
of water intoxication cannot be ruled out.
It is usually taught that hypernatremia should be
corrected slowly, while, if symptomatic (seizures,
lethargy, etc.), hyponatremia can be corrected
quickly. However, if the history suggests that the
hyponatremia may be long standing, it may be prudent
to correct the hyponatremia slowly (if the patient is not
severely symptomatic) to prevent rapid fluid shifts
between the intracellular and extracellular
compartments that have been accustomed to a low
sodium environment. This would be difficult to prove
since such severe long standing hyponatremia is very
uncommon.
References
Bays J. Child Abuse by Poisoning. In: Reece RM.
Child Abuse: Medical Diagnosis and Management.
Philadelphia, Lea & Febinger, 1994, pp. 88-89.
Morimer JG. Acute Water Intoxication as Another
Unusual Manifestation of Child Abuse. Arch Dis Child
1980:55:401-403.
Keating JP, Schears GJ, Dodge PR. Oral Water
Intoxication in Infants - An American Epidemic. Am J
Dis Child 1991;145:985-990.
This CT scan shows a 2.5cm cystic partially calcified
suprasellar mass which undergoes peripheral
enhancement with contrast. This is most likely a
craniopharyngioma. Other structures such as the
tentorium are also enhancing.
His non-reactive pupils are due to erosion of the
optic nerves. His fundoscopic findings are due to
severe optic atrophy. It is difficult to believe that the
child's family could not tell that he was blind. His motor
and developmental delays are now well explained. It is
amazing that this child could walk around. It is not
surprising that he would bump into the walls since he
could not see.
His severe hyponatremia is probably longstanding.
Only a child with chronic hyponatremia would be able to
tolerate such a low sodium value of 97 mEq/liter.
Although this patient probably had long standing
panhypopituitarism it is unclear why both his growth
and his glucose homeostasis were satisfactory.
One would expect that he should have growth hormone
deficiency and insufficient adrenal stimulation.
Diabetes insipidus would not account for his
hyponatremia since diabetes insipidus should result in
hypernatremia. Hypoaldosteronism coupled with
SIADH could explain this, but this degree of
hyponatremia is so severe that a concomitant element
of water intoxication cannot be ruled out.
It is usually taught that hypernatremia should be
corrected slowly, while, if symptomatic (seizures,
lethargy, etc.), hyponatremia can be corrected
quickly. However, if the history suggests that the
hyponatremia may be long standing, it may be prudent
to correct the hyponatremia slowly (if the patient is not
severely symptomatic) to prevent rapid fluid shifts
between the intracellular and extracellular
compartments that have been accustomed to a low
sodium environment. This would be difficult to prove
since such severe long standing hyponatremia is very
uncommon.
References
Bays J. Child Abuse by Poisoning. In: Reece RM.
Child Abuse: Medical Diagnosis and Management.
Philadelphia, Lea & Febinger, 1994, pp. 88-89.
Morimer JG. Acute Water Intoxication as Another
Unusual Manifestation of Child Abuse. Arch Dis Child
1980:55:401-403.
Keating JP, Schears GJ, Dodge PR. Oral Water
Intoxication in Infants - An American Epidemic. Am J
Dis Child 1991;145:985-990.
Return to Radiology Cases In Ped Emerg Med Case Selection Page
Return to Univ. Hawaii Dept. Pediatrics Home Page
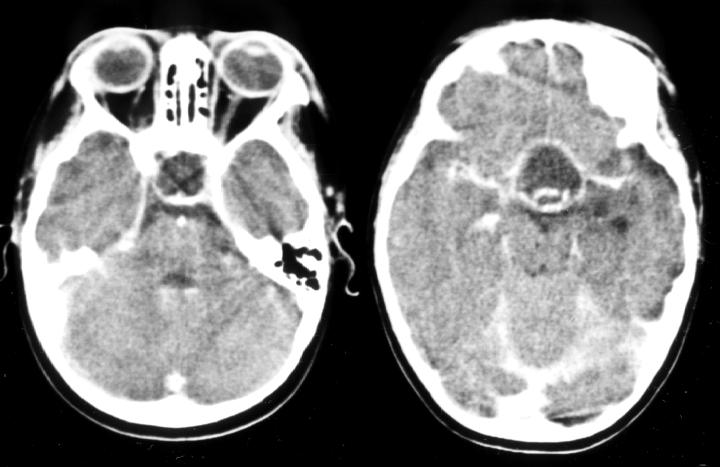 This CT scan shows a 2.5cm cystic partially calcified
suprasellar mass which undergoes peripheral
enhancement with contrast. This is most likely a
craniopharyngioma. Other structures such as the
tentorium are also enhancing.
His non-reactive pupils are due to erosion of the
optic nerves. His fundoscopic findings are due to
severe optic atrophy. It is difficult to believe that the
child's family could not tell that he was blind. His motor
and developmental delays are now well explained. It is
amazing that this child could walk around. It is not
surprising that he would bump into the walls since he
could not see.
His severe hyponatremia is probably longstanding.
Only a child with chronic hyponatremia would be able to
tolerate such a low sodium value of 97 mEq/liter.
Although this patient probably had long standing
panhypopituitarism it is unclear why both his growth
and his glucose homeostasis were satisfactory.
One would expect that he should have growth hormone
deficiency and insufficient adrenal stimulation.
Diabetes insipidus would not account for his
hyponatremia since diabetes insipidus should result in
hypernatremia. Hypoaldosteronism coupled with
SIADH could explain this, but this degree of
hyponatremia is so severe that a concomitant element
of water intoxication cannot be ruled out.
It is usually taught that hypernatremia should be
corrected slowly, while, if symptomatic (seizures,
lethargy, etc.), hyponatremia can be corrected
quickly. However, if the history suggests that the
hyponatremia may be long standing, it may be prudent
to correct the hyponatremia slowly (if the patient is not
severely symptomatic) to prevent rapid fluid shifts
between the intracellular and extracellular
compartments that have been accustomed to a low
sodium environment. This would be difficult to prove
since such severe long standing hyponatremia is very
uncommon.
References
Bays J. Child Abuse by Poisoning. In: Reece RM.
Child Abuse: Medical Diagnosis and Management.
Philadelphia, Lea & Febinger, 1994, pp. 88-89.
Morimer JG. Acute Water Intoxication as Another
Unusual Manifestation of Child Abuse. Arch Dis Child
1980:55:401-403.
Keating JP, Schears GJ, Dodge PR. Oral Water
Intoxication in Infants - An American Epidemic. Am J
Dis Child 1991;145:985-990.
This CT scan shows a 2.5cm cystic partially calcified
suprasellar mass which undergoes peripheral
enhancement with contrast. This is most likely a
craniopharyngioma. Other structures such as the
tentorium are also enhancing.
His non-reactive pupils are due to erosion of the
optic nerves. His fundoscopic findings are due to
severe optic atrophy. It is difficult to believe that the
child's family could not tell that he was blind. His motor
and developmental delays are now well explained. It is
amazing that this child could walk around. It is not
surprising that he would bump into the walls since he
could not see.
His severe hyponatremia is probably longstanding.
Only a child with chronic hyponatremia would be able to
tolerate such a low sodium value of 97 mEq/liter.
Although this patient probably had long standing
panhypopituitarism it is unclear why both his growth
and his glucose homeostasis were satisfactory.
One would expect that he should have growth hormone
deficiency and insufficient adrenal stimulation.
Diabetes insipidus would not account for his
hyponatremia since diabetes insipidus should result in
hypernatremia. Hypoaldosteronism coupled with
SIADH could explain this, but this degree of
hyponatremia is so severe that a concomitant element
of water intoxication cannot be ruled out.
It is usually taught that hypernatremia should be
corrected slowly, while, if symptomatic (seizures,
lethargy, etc.), hyponatremia can be corrected
quickly. However, if the history suggests that the
hyponatremia may be long standing, it may be prudent
to correct the hyponatremia slowly (if the patient is not
severely symptomatic) to prevent rapid fluid shifts
between the intracellular and extracellular
compartments that have been accustomed to a low
sodium environment. This would be difficult to prove
since such severe long standing hyponatremia is very
uncommon.
References
Bays J. Child Abuse by Poisoning. In: Reece RM.
Child Abuse: Medical Diagnosis and Management.
Philadelphia, Lea & Febinger, 1994, pp. 88-89.
Morimer JG. Acute Water Intoxication as Another
Unusual Manifestation of Child Abuse. Arch Dis Child
1980:55:401-403.
Keating JP, Schears GJ, Dodge PR. Oral Water
Intoxication in Infants - An American Epidemic. Am J
Dis Child 1991;145:985-990.