Fever with Neck Stiffness...Rule-Out Meningitis?
Radiology Cases in Pediatric Emergency Medicine
Volume 5, Case 1
Alson S. Inaba, MD
Kapiolani Medical Center For Women And Children
University of Hawaii John A. Burns School of Medicine
A 7 year-old male is referred to the Emergency
Department (ED) with fever and neck stiffness. Four
days prior to this ED referral, he had come home from
school complaining of a bad headache, nausea, sore
throat and "neck pain." He denied any history of neck
or oropharyngeal trauma. He was seen by his
pediatrician and was noted to have a temperature of
40.1 C. He was diagnosed as probably having the "flu,"
and was told to drink a lot of fluids and to take
acetaminophen for his fever. He was again seen by his
pediatrician today because of persistent fever, neck
pain and he was also now complaining of a stiff neck.
He was thus referred to the ED as a rule-out meningitis
case.
Upon presentation to the ED he is slightly
tired-appearing, but non-toxic. His vital signs are within
normal limits with the exception of a temperature of
39.0 C. His airway is patent without any stridor,
dysphagia or drooling. His tonsils are 2+ enlarged
bilaterally with mild erythema but no exudates. The
uvula is midline and there is no obvious "muffled"
quality to this voice. There is no obvious "bulging" of
his retropharynx and he does not exhibit any trismus.
He has a few 1 cm, tender cervical nodes bilaterally and
both the Brudzinski's and Kernig's signs are negative.
Although he does not complain of any neck pain with
active neck flexion, he does complain of posterior neck
pain upon active neck extension. Palpation over the
posterior aspect of his neck fails to reveal any areas of
point tenderness. The remainder of his physical
examination is within normal limits.
A lumbar puncture is performed which reveals 1
WBC and 1 RBC with normal protein and glucose
values and no organisms seen on the gram stain. On
repeat examination, he still seems to complain of
posterior neck pain with active neck extension. A
lateral neck radiograph is then obtained.
View lateral neck radiograph.
 Based on your interpretation of this lateral neck
radiograph, what is your tentative diagnosis and what
would you do to further evaluate and manage this
disease entity?
Radiologic Discussion:
The prevertebral space and the retropharyngeal
space are two distinct spaces. The retropharyngeal
space extends from the base of the skull down to the
level of the carina, and is located between the
buccopharyngeal mucosa and the prevertebral fascia.
The prevertebral space is a potential space that is
located between the anterior aspect of the vertebral
body and the prevertebral fascia.
When one suspects the possibility of a
retropharyngeal infection (i.e., cellulitis vs. abscess), a
lateral neck radiograph should be obtained to evaluate
the prevertebral soft tissue thickness and contour. The
optimal technique to accurately assess the prevertebral
soft tissues is to have the patient's neck in the extended
position and to obtain the radiograph during
end-INSPiration. If the patient's neck is flexed and/or if
the radiograph is obtained during end-EXPiration the
prevertebral soft tissues may appear falsely widened
and thus give the false impression of a possible
retropharyngeal infection (RPI).
View a false positive radiograph.
Based on your interpretation of this lateral neck
radiograph, what is your tentative diagnosis and what
would you do to further evaluate and manage this
disease entity?
Radiologic Discussion:
The prevertebral space and the retropharyngeal
space are two distinct spaces. The retropharyngeal
space extends from the base of the skull down to the
level of the carina, and is located between the
buccopharyngeal mucosa and the prevertebral fascia.
The prevertebral space is a potential space that is
located between the anterior aspect of the vertebral
body and the prevertebral fascia.
When one suspects the possibility of a
retropharyngeal infection (i.e., cellulitis vs. abscess), a
lateral neck radiograph should be obtained to evaluate
the prevertebral soft tissue thickness and contour. The
optimal technique to accurately assess the prevertebral
soft tissues is to have the patient's neck in the extended
position and to obtain the radiograph during
end-INSPiration. If the patient's neck is flexed and/or if
the radiograph is obtained during end-EXPiration the
prevertebral soft tissues may appear falsely widened
and thus give the false impression of a possible
retropharyngeal infection (RPI).
View a false positive radiograph.
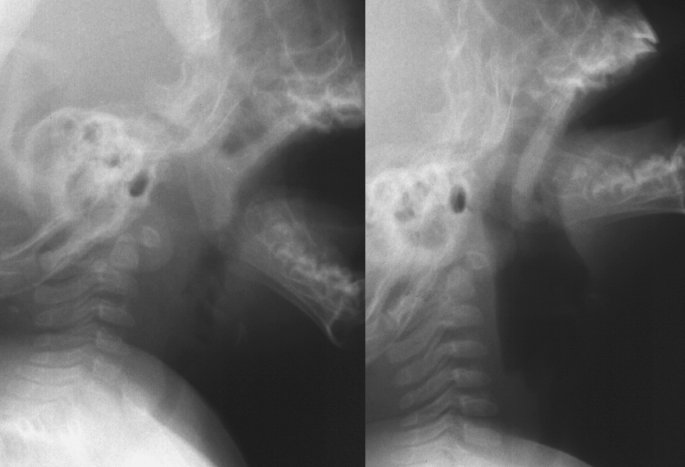 In the image on the left, the prevertebral soft tissues
appear to be widened on this initial view. However this
view was obtained with the neck in a neutral position
and during end-EXPiration. The image on the right is
the same patient, obtained with the neck extended
(lordotic) during end-INSPiration, which demonstrates
that the prevertebral soft tissues are actually normal.
Note that the previously widened prevertebral soft
tissues have now resolved with proper positioning.
View another example of positioning.
In the image on the left, the prevertebral soft tissues
appear to be widened on this initial view. However this
view was obtained with the neck in a neutral position
and during end-EXPiration. The image on the right is
the same patient, obtained with the neck extended
(lordotic) during end-INSPiration, which demonstrates
that the prevertebral soft tissues are actually normal.
Note that the previously widened prevertebral soft
tissues have now resolved with proper positioning.
View another example of positioning.
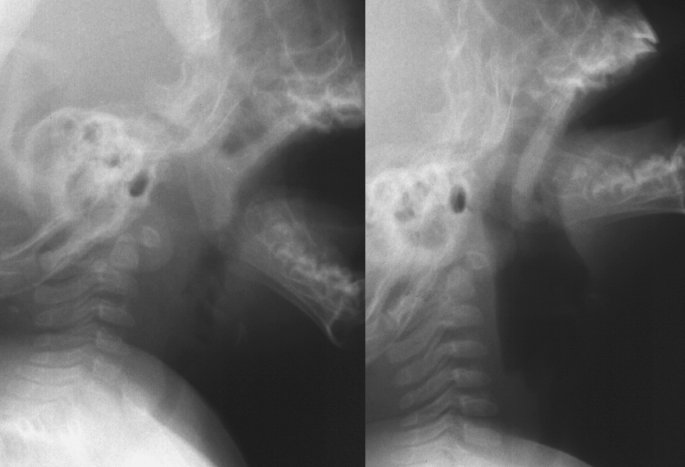
 This pair of lateral neck radiographs shows
prevertebral soft tissue widening on the left image. The
image on the right shows the same patient with
extension of the neck and persistence of the
prevertebral soft tissue widening. In this case, the
prevertebral soft tissue widening is true.
Other causes of widening of the prevertebral soft
tissue space include a mass (neoplastic or other
causes) or hemorrhage from an occult cervical spine
fracture.
When attempting to evaluate the thickness of the
prevertebral soft tissues on the lateral neck view, there
are several methods and factors to keep in mind:
a) The normal thickness of the prevertebral soft
tissues on the lateral neck view is usually < 7 mm
anterior to C2 and < 5 mm anterior to C3/C4 (or less
than half the diameter of the vertebral bodies).
Although these absolute measurements can be
utilized to assess the thickness of the prevertebral soft
tissues, there are several other factors that should also
be considered when evaluating the lateral neck
radiograph. The absolute measurement/thickness of
the prevertebral soft tissues is not the only criteria to
use when attempting to determine if a retropharyngeal
infection is present.
b) On the lateral neck radiograph, there normally is
a "step-off" between the posterior wall of the pharynx
and the posterior wall of the trachea at the level of the
larynx (approximately at the level of C4).
View "step-off".
This pair of lateral neck radiographs shows
prevertebral soft tissue widening on the left image. The
image on the right shows the same patient with
extension of the neck and persistence of the
prevertebral soft tissue widening. In this case, the
prevertebral soft tissue widening is true.
Other causes of widening of the prevertebral soft
tissue space include a mass (neoplastic or other
causes) or hemorrhage from an occult cervical spine
fracture.
When attempting to evaluate the thickness of the
prevertebral soft tissues on the lateral neck view, there
are several methods and factors to keep in mind:
a) The normal thickness of the prevertebral soft
tissues on the lateral neck view is usually < 7 mm
anterior to C2 and < 5 mm anterior to C3/C4 (or less
than half the diameter of the vertebral bodies).
Although these absolute measurements can be
utilized to assess the thickness of the prevertebral soft
tissues, there are several other factors that should also
be considered when evaluating the lateral neck
radiograph. The absolute measurement/thickness of
the prevertebral soft tissues is not the only criteria to
use when attempting to determine if a retropharyngeal
infection is present.
b) On the lateral neck radiograph, there normally is
a "step-off" between the posterior wall of the pharynx
and the posterior wall of the trachea at the level of the
larynx (approximately at the level of C4).
View "step-off".
 The vertical black lines demonstrate the "step-off" in
this patient with croup (subglottic narrowing) and a
normal prevertebral soft tissue region. The upper mark
is in line with the posterior wall of the pharynx while the
lower mark is in line with the posterior wall of the
trachea. The superior-most aspect of the esophagus
normally begins approximately at the level of C4, and
thus normally, the posterior wall of the trachea at this
level should NOT be in alignment with the posterior
pharyngeal wall. When this normal step-off is ABSENT,
one should suspect a possible retropharyngeal
inflammatory process (above the level of C4) which is
causing the posterior pharyngeal wall to be displaced
anteriorly to now be in alignment with the posterior wall
of the tracheal air shadow. Note that this "step-off" is
blunted or absent in the patient with a retropharyngeal
infection. Examine the earlier radiographs again.
The vertical black lines demonstrate the "step-off" in
this patient with croup (subglottic narrowing) and a
normal prevertebral soft tissue region. The upper mark
is in line with the posterior wall of the pharynx while the
lower mark is in line with the posterior wall of the
trachea. The superior-most aspect of the esophagus
normally begins approximately at the level of C4, and
thus normally, the posterior wall of the trachea at this
level should NOT be in alignment with the posterior
pharyngeal wall. When this normal step-off is ABSENT,
one should suspect a possible retropharyngeal
inflammatory process (above the level of C4) which is
causing the posterior pharyngeal wall to be displaced
anteriorly to now be in alignment with the posterior wall
of the tracheal air shadow. Note that this "step-off" is
blunted or absent in the patient with a retropharyngeal
infection. Examine the earlier radiographs again.

 c) Normally the air-soft tissue interface between the
prevertebral soft tissue and the air in the posterior
pharynx should be very sharp. Any inflammatory
process of the retropharyngeal space creates an
"indistinctness" and irregularity of this air-soft tissue
interface.
d) The contour of the prevertebral soft tissue should
normally follow the contour of the anterior aspect of the
cervical vertebrae.
Based on the above discussion, how would you
interpret the lateral neck radiograph of the patient
discussed above?
View lateral neck.
c) Normally the air-soft tissue interface between the
prevertebral soft tissue and the air in the posterior
pharynx should be very sharp. Any inflammatory
process of the retropharyngeal space creates an
"indistinctness" and irregularity of this air-soft tissue
interface.
d) The contour of the prevertebral soft tissue should
normally follow the contour of the anterior aspect of the
cervical vertebrae.
Based on the above discussion, how would you
interpret the lateral neck radiograph of the patient
discussed above?
View lateral neck.
 Radiologist's interpretation: The lateral neck
radiograph reveals a moderate degree of soft tissue
swelling of the prevertebral/retropharyngeal soft tissues.
When the lateral neck radiograph suggests a
retropharyngeal infection, a CT scan of the neck should
be obtained to:
a) Delineate the extent of the infection (i.e., how far
down the pharynx, neck and chest does the infectious
process extend?).
b) Attempt to differentiate between a
retropharyngeal cellulitis/phlegmon versus a
retropharyngeal abscess.
Two characteristic findings that are suggestive of
an abscess are:
a) A rim of enhancement around a hypodense mass.
b) A convex appearance ("bulging-appearance") of
the surface of the hypodense mass. In contrast to this,
a phlegmon (pyogenic cellulitis) typically does not have
a rim of enhancement around the hypodense mass and
the surfaces of the phlegmon do not typically exhibit a
convex appearance.
A neck CT scan (with IV contrast) is obtained on the
patient discussed above. Based on the above
discussion, how would you interpret this patient's neck
CT scan?
View CT.
Radiologist's interpretation: The lateral neck
radiograph reveals a moderate degree of soft tissue
swelling of the prevertebral/retropharyngeal soft tissues.
When the lateral neck radiograph suggests a
retropharyngeal infection, a CT scan of the neck should
be obtained to:
a) Delineate the extent of the infection (i.e., how far
down the pharynx, neck and chest does the infectious
process extend?).
b) Attempt to differentiate between a
retropharyngeal cellulitis/phlegmon versus a
retropharyngeal abscess.
Two characteristic findings that are suggestive of
an abscess are:
a) A rim of enhancement around a hypodense mass.
b) A convex appearance ("bulging-appearance") of
the surface of the hypodense mass. In contrast to this,
a phlegmon (pyogenic cellulitis) typically does not have
a rim of enhancement around the hypodense mass and
the surfaces of the phlegmon do not typically exhibit a
convex appearance.
A neck CT scan (with IV contrast) is obtained on the
patient discussed above. Based on the above
discussion, how would you interpret this patient's neck
CT scan?
View CT.
 Radiologist's interpretation: There is a slight degree
of thickening of the prevertebral/retropharyngeal
soft-tissues. There is a plaque-like area of hypodensity
(arrow) anterior to the vertebral bodies and the longus
colli muscles which probably represents a fluid
collection in the retropharyngeal soft tissues without
definite abscess formation.
This case is most consistent with a retropharyngeal
phlegmon (pyogenic cellulitis) rather than a true
absence. There is no rim of enhancement (with
contrast) around the lesion and the soft tissues do not
bulge anteriorly in a convex fashion.
View abscess example.
Radiologist's interpretation: There is a slight degree
of thickening of the prevertebral/retropharyngeal
soft-tissues. There is a plaque-like area of hypodensity
(arrow) anterior to the vertebral bodies and the longus
colli muscles which probably represents a fluid
collection in the retropharyngeal soft tissues without
definite abscess formation.
This case is most consistent with a retropharyngeal
phlegmon (pyogenic cellulitis) rather than a true
absence. There is no rim of enhancement (with
contrast) around the lesion and the soft tissues do not
bulge anteriorly in a convex fashion.
View abscess example.
 This CT scan (with contrast) shows CT findings
more consistent with an abscess rather than a
phlegmon. Note the larger size, the rim of contrast
enhancement around the lesion and the anterior bulging
(convexity) of the prevertebral soft tissues. These
findings are suggestive of an abscess.
Discussion:
Retropharyngeal abscesses are the second most
common of the deep neck infections in children (second
only to peritonsillar abscesses which account for up to
50% of the deep neck infections in the pediatric
population).
The most common pathophysiologic etiology of a
retropharyngeal abscess is via suppurative adenitis of
the paramedian chains of lymphoid tissue (that drain
the nasopharynx, adenoids and posterior paranasal
sinuses) located in the retropharyngeal space. Thus,
otitis media and nasopharyngeal infections may lead to
suppuration of these paramedian chains of lymphoid
tissue and result in a retropharyngeal abscess.
Because this paramedian lymph tissue usually begins
to atrophy during the third to fourth year of life, it is no
surprise that the majority of retropharyngeal abscess
cases (50%) occur in children 6-12 months of age, with
96% of the cases occurring in children < 6 years of age.
Two other pathophysiologic etiologies of
retropharyngeal abscesses are via: 1) Direct
penetrating trauma to the retropharyngeal space (i.e., a
child who falls with a popsicle stick in his mouth and
sustains direct penetration of the posterior pharynx),
and 2) Anterior extension of a vertebral osteomyelitis
into the pre-vertebral soft tissue space.
A child with a retropharyngeal infection may present
with fever, sore throat, dysphagia and/or neck pain. If
the retropharyngeal infection is significant enough to
begin to compromise the patency of the child's posterior
pharynx, the patient may also present in a toxic fashion
with drooling and stridor (and thus mimicking the
presentation of a child with epiglottitis or croup). A child
with a retropharyngeal abscess may also present with
meningeal signs such as neck pain/stiffness secondary
to irritation of the paravertebral ligaments. Although
many textbooks comment on the fact that the posterior
pharynx of a child with a retropharyngeal abscess may
appear to be "bulging", in my personal experience this
physical examination finding has not been very obvious
in children with very early retropharyngeal infections
(i.e., cellulitis / phlegmon). Anterior deviation of the
uvula may also be present in a child with a
retropharyngeal infection. Examination of the
oropharynx should also be deferred if the child with a
possible retropharyngeal abscess presents in a
dramatic fashion with drooling and stridor.
Complications of a retropharyngeal abscess include:
1) Acute airway obstruction via obstruction of the
posterior pharynx.
2) Aspiration secondary to the child's inability to
handle his/her own oral secretions.
3) Rupture of the abscess into the pharynx resulting
in aspiration.
4) Extension of the abscess causing mediastinitis,
pneumonia or necrotizing fasciitis.
5) Sepsis
6) Dehydration secondary to the child's inability to
tolerate oral fluids.
The two most common organisms recovered from
retropharyngeal abscess cultures are Staphylococcus
aureus and Group A beta-hemolytic Streptococcus. A
child with a retropharyngeal cellulitis should be
hospitalized for intravenous antibiotics and observation
for potential airway compromise. If a retropharyngeal
abscess is diagnosed on the neck CT scan, the child
will also require surgical drainage of the abscess in
addition to intravenous antibiotics. Empiric antibiotic
regimens for a child with a retropharyngeal abscess
should cover for Staphylococcus aureus, Group A
beta-hemolytic Streptococcus and anaerobes (i.e.,
Bacteroides). Options include: oxacillin, first
generation cephalosporins, and/or clindamycin.
Consider the empiric use of vancomycin to cover the
possibility of methicillin resistant Staph aureus (MRSA).
Should this possibility materialize, sepsis may result
without adequate coverage.
Post-discussion quiz questions:
1) The majority of retropharyngeal abscess cases
occur in which age group?
a) < 1 year of age
b) 2 - 6 years of age
c) 7 - 10 years of age
d) > 12 years of age
2) List the three pathophysiologic mechanisms which
are responsible for producing a retropharyngeal
abscess:
a)
b)
c)
3) What are the two most common organisms that are
recovered from retropharyngeal abscess cultures?
a)
b)
4) The radiographic technique to optimally visualize the
prevertebral soft tissues on the lateral neck view is
during:
a) End-INSPiration with the patient's neck in the
flexed position.
b) End-EXPiration with the patient's neck in the
flexed position.
c) End-INSPiration with the patient's neck in the
extended position.
d) End-EXPiration with the patient's neck in the
flexed position.
5) List at least 3 potential complications of a
retropharyngeal abscess:
a)
b)
c)
References:
Abrunzo TJ, Santamaria JP. Peritonsillar Abscess
and Retropharyngeal Abscess. In: Strange GR, et al.
Pediatric Emergency Medicine: A Comprehensive
Study Guide. New York, McGraw-Hill; pp. 414-416,
1996.
Harris JH, et al. Radiographic Anatomy of the Neck.
In: The Radiology of Emergency Medicine (Third
Edition). Baltimore, Williams & Wilkins; pp. 133-138,
1993.
Sanatamaria JP, Abrunzo TJ. Peritonsillar Abscess
and Retropharyngeal Abscess. In: Barkin RA, et al.
Pediatric Emergency Medicine: Concepts and Clinical
Practice. St Louis, Mosby Year Book; pp. 679-681,
1992.
Swischuk LE. Retropharyngeal Abscess. In:
Emergency Imaging of the Acutely Ill or Injured Child
(Third Edition). Baltimore, Williams & Wilkins; pp.
171-175, 1994.
This CT scan (with contrast) shows CT findings
more consistent with an abscess rather than a
phlegmon. Note the larger size, the rim of contrast
enhancement around the lesion and the anterior bulging
(convexity) of the prevertebral soft tissues. These
findings are suggestive of an abscess.
Discussion:
Retropharyngeal abscesses are the second most
common of the deep neck infections in children (second
only to peritonsillar abscesses which account for up to
50% of the deep neck infections in the pediatric
population).
The most common pathophysiologic etiology of a
retropharyngeal abscess is via suppurative adenitis of
the paramedian chains of lymphoid tissue (that drain
the nasopharynx, adenoids and posterior paranasal
sinuses) located in the retropharyngeal space. Thus,
otitis media and nasopharyngeal infections may lead to
suppuration of these paramedian chains of lymphoid
tissue and result in a retropharyngeal abscess.
Because this paramedian lymph tissue usually begins
to atrophy during the third to fourth year of life, it is no
surprise that the majority of retropharyngeal abscess
cases (50%) occur in children 6-12 months of age, with
96% of the cases occurring in children < 6 years of age.
Two other pathophysiologic etiologies of
retropharyngeal abscesses are via: 1) Direct
penetrating trauma to the retropharyngeal space (i.e., a
child who falls with a popsicle stick in his mouth and
sustains direct penetration of the posterior pharynx),
and 2) Anterior extension of a vertebral osteomyelitis
into the pre-vertebral soft tissue space.
A child with a retropharyngeal infection may present
with fever, sore throat, dysphagia and/or neck pain. If
the retropharyngeal infection is significant enough to
begin to compromise the patency of the child's posterior
pharynx, the patient may also present in a toxic fashion
with drooling and stridor (and thus mimicking the
presentation of a child with epiglottitis or croup). A child
with a retropharyngeal abscess may also present with
meningeal signs such as neck pain/stiffness secondary
to irritation of the paravertebral ligaments. Although
many textbooks comment on the fact that the posterior
pharynx of a child with a retropharyngeal abscess may
appear to be "bulging", in my personal experience this
physical examination finding has not been very obvious
in children with very early retropharyngeal infections
(i.e., cellulitis / phlegmon). Anterior deviation of the
uvula may also be present in a child with a
retropharyngeal infection. Examination of the
oropharynx should also be deferred if the child with a
possible retropharyngeal abscess presents in a
dramatic fashion with drooling and stridor.
Complications of a retropharyngeal abscess include:
1) Acute airway obstruction via obstruction of the
posterior pharynx.
2) Aspiration secondary to the child's inability to
handle his/her own oral secretions.
3) Rupture of the abscess into the pharynx resulting
in aspiration.
4) Extension of the abscess causing mediastinitis,
pneumonia or necrotizing fasciitis.
5) Sepsis
6) Dehydration secondary to the child's inability to
tolerate oral fluids.
The two most common organisms recovered from
retropharyngeal abscess cultures are Staphylococcus
aureus and Group A beta-hemolytic Streptococcus. A
child with a retropharyngeal cellulitis should be
hospitalized for intravenous antibiotics and observation
for potential airway compromise. If a retropharyngeal
abscess is diagnosed on the neck CT scan, the child
will also require surgical drainage of the abscess in
addition to intravenous antibiotics. Empiric antibiotic
regimens for a child with a retropharyngeal abscess
should cover for Staphylococcus aureus, Group A
beta-hemolytic Streptococcus and anaerobes (i.e.,
Bacteroides). Options include: oxacillin, first
generation cephalosporins, and/or clindamycin.
Consider the empiric use of vancomycin to cover the
possibility of methicillin resistant Staph aureus (MRSA).
Should this possibility materialize, sepsis may result
without adequate coverage.
Post-discussion quiz questions:
1) The majority of retropharyngeal abscess cases
occur in which age group?
a) < 1 year of age
b) 2 - 6 years of age
c) 7 - 10 years of age
d) > 12 years of age
2) List the three pathophysiologic mechanisms which
are responsible for producing a retropharyngeal
abscess:
a)
b)
c)
3) What are the two most common organisms that are
recovered from retropharyngeal abscess cultures?
a)
b)
4) The radiographic technique to optimally visualize the
prevertebral soft tissues on the lateral neck view is
during:
a) End-INSPiration with the patient's neck in the
flexed position.
b) End-EXPiration with the patient's neck in the
flexed position.
c) End-INSPiration with the patient's neck in the
extended position.
d) End-EXPiration with the patient's neck in the
flexed position.
5) List at least 3 potential complications of a
retropharyngeal abscess:
a)
b)
c)
References:
Abrunzo TJ, Santamaria JP. Peritonsillar Abscess
and Retropharyngeal Abscess. In: Strange GR, et al.
Pediatric Emergency Medicine: A Comprehensive
Study Guide. New York, McGraw-Hill; pp. 414-416,
1996.
Harris JH, et al. Radiographic Anatomy of the Neck.
In: The Radiology of Emergency Medicine (Third
Edition). Baltimore, Williams & Wilkins; pp. 133-138,
1993.
Sanatamaria JP, Abrunzo TJ. Peritonsillar Abscess
and Retropharyngeal Abscess. In: Barkin RA, et al.
Pediatric Emergency Medicine: Concepts and Clinical
Practice. St Louis, Mosby Year Book; pp. 679-681,
1992.
Swischuk LE. Retropharyngeal Abscess. In:
Emergency Imaging of the Acutely Ill or Injured Child
(Third Edition). Baltimore, Williams & Wilkins; pp.
171-175, 1994.
Return to Radiology Cases In Ped Emerg Med Case Selection Page
Return to Univ. Hawaii Dept. Pediatrics Home Page
 Based on your interpretation of this lateral neck
radiograph, what is your tentative diagnosis and what
would you do to further evaluate and manage this
disease entity?
Radiologic Discussion:
The prevertebral space and the retropharyngeal
space are two distinct spaces. The retropharyngeal
space extends from the base of the skull down to the
level of the carina, and is located between the
buccopharyngeal mucosa and the prevertebral fascia.
The prevertebral space is a potential space that is
located between the anterior aspect of the vertebral
body and the prevertebral fascia.
When one suspects the possibility of a
retropharyngeal infection (i.e., cellulitis vs. abscess), a
lateral neck radiograph should be obtained to evaluate
the prevertebral soft tissue thickness and contour. The
optimal technique to accurately assess the prevertebral
soft tissues is to have the patient's neck in the extended
position and to obtain the radiograph during
end-INSPiration. If the patient's neck is flexed and/or if
the radiograph is obtained during end-EXPiration the
prevertebral soft tissues may appear falsely widened
and thus give the false impression of a possible
retropharyngeal infection (RPI).
View a false positive radiograph.
Based on your interpretation of this lateral neck
radiograph, what is your tentative diagnosis and what
would you do to further evaluate and manage this
disease entity?
Radiologic Discussion:
The prevertebral space and the retropharyngeal
space are two distinct spaces. The retropharyngeal
space extends from the base of the skull down to the
level of the carina, and is located between the
buccopharyngeal mucosa and the prevertebral fascia.
The prevertebral space is a potential space that is
located between the anterior aspect of the vertebral
body and the prevertebral fascia.
When one suspects the possibility of a
retropharyngeal infection (i.e., cellulitis vs. abscess), a
lateral neck radiograph should be obtained to evaluate
the prevertebral soft tissue thickness and contour. The
optimal technique to accurately assess the prevertebral
soft tissues is to have the patient's neck in the extended
position and to obtain the radiograph during
end-INSPiration. If the patient's neck is flexed and/or if
the radiograph is obtained during end-EXPiration the
prevertebral soft tissues may appear falsely widened
and thus give the false impression of a possible
retropharyngeal infection (RPI).
View a false positive radiograph.
 In the image on the left, the prevertebral soft tissues
appear to be widened on this initial view. However this
view was obtained with the neck in a neutral position
and during end-EXPiration. The image on the right is
the same patient, obtained with the neck extended
(lordotic) during end-INSPiration, which demonstrates
that the prevertebral soft tissues are actually normal.
Note that the previously widened prevertebral soft
tissues have now resolved with proper positioning.
View another example of positioning.
In the image on the left, the prevertebral soft tissues
appear to be widened on this initial view. However this
view was obtained with the neck in a neutral position
and during end-EXPiration. The image on the right is
the same patient, obtained with the neck extended
(lordotic) during end-INSPiration, which demonstrates
that the prevertebral soft tissues are actually normal.
Note that the previously widened prevertebral soft
tissues have now resolved with proper positioning.
View another example of positioning.
 This pair of lateral neck radiographs shows
prevertebral soft tissue widening on the left image. The
image on the right shows the same patient with
extension of the neck and persistence of the
prevertebral soft tissue widening. In this case, the
prevertebral soft tissue widening is true.
Other causes of widening of the prevertebral soft
tissue space include a mass (neoplastic or other
causes) or hemorrhage from an occult cervical spine
fracture.
When attempting to evaluate the thickness of the
prevertebral soft tissues on the lateral neck view, there
are several methods and factors to keep in mind:
a) The normal thickness of the prevertebral soft
tissues on the lateral neck view is usually < 7 mm
anterior to C2 and < 5 mm anterior to C3/C4 (or less
than half the diameter of the vertebral bodies).
Although these absolute measurements can be
utilized to assess the thickness of the prevertebral soft
tissues, there are several other factors that should also
be considered when evaluating the lateral neck
radiograph. The absolute measurement/thickness of
the prevertebral soft tissues is not the only criteria to
use when attempting to determine if a retropharyngeal
infection is present.
b) On the lateral neck radiograph, there normally is
a "step-off" between the posterior wall of the pharynx
and the posterior wall of the trachea at the level of the
larynx (approximately at the level of C4).
View "step-off".
This pair of lateral neck radiographs shows
prevertebral soft tissue widening on the left image. The
image on the right shows the same patient with
extension of the neck and persistence of the
prevertebral soft tissue widening. In this case, the
prevertebral soft tissue widening is true.
Other causes of widening of the prevertebral soft
tissue space include a mass (neoplastic or other
causes) or hemorrhage from an occult cervical spine
fracture.
When attempting to evaluate the thickness of the
prevertebral soft tissues on the lateral neck view, there
are several methods and factors to keep in mind:
a) The normal thickness of the prevertebral soft
tissues on the lateral neck view is usually < 7 mm
anterior to C2 and < 5 mm anterior to C3/C4 (or less
than half the diameter of the vertebral bodies).
Although these absolute measurements can be
utilized to assess the thickness of the prevertebral soft
tissues, there are several other factors that should also
be considered when evaluating the lateral neck
radiograph. The absolute measurement/thickness of
the prevertebral soft tissues is not the only criteria to
use when attempting to determine if a retropharyngeal
infection is present.
b) On the lateral neck radiograph, there normally is
a "step-off" between the posterior wall of the pharynx
and the posterior wall of the trachea at the level of the
larynx (approximately at the level of C4).
View "step-off".
 The vertical black lines demonstrate the "step-off" in
this patient with croup (subglottic narrowing) and a
normal prevertebral soft tissue region. The upper mark
is in line with the posterior wall of the pharynx while the
lower mark is in line with the posterior wall of the
trachea. The superior-most aspect of the esophagus
normally begins approximately at the level of C4, and
thus normally, the posterior wall of the trachea at this
level should NOT be in alignment with the posterior
pharyngeal wall. When this normal step-off is ABSENT,
one should suspect a possible retropharyngeal
inflammatory process (above the level of C4) which is
causing the posterior pharyngeal wall to be displaced
anteriorly to now be in alignment with the posterior wall
of the tracheal air shadow. Note that this "step-off" is
blunted or absent in the patient with a retropharyngeal
infection. Examine the earlier radiographs again.
The vertical black lines demonstrate the "step-off" in
this patient with croup (subglottic narrowing) and a
normal prevertebral soft tissue region. The upper mark
is in line with the posterior wall of the pharynx while the
lower mark is in line with the posterior wall of the
trachea. The superior-most aspect of the esophagus
normally begins approximately at the level of C4, and
thus normally, the posterior wall of the trachea at this
level should NOT be in alignment with the posterior
pharyngeal wall. When this normal step-off is ABSENT,
one should suspect a possible retropharyngeal
inflammatory process (above the level of C4) which is
causing the posterior pharyngeal wall to be displaced
anteriorly to now be in alignment with the posterior wall
of the tracheal air shadow. Note that this "step-off" is
blunted or absent in the patient with a retropharyngeal
infection. Examine the earlier radiographs again.

 c) Normally the air-soft tissue interface between the
prevertebral soft tissue and the air in the posterior
pharynx should be very sharp. Any inflammatory
process of the retropharyngeal space creates an
"indistinctness" and irregularity of this air-soft tissue
interface.
d) The contour of the prevertebral soft tissue should
normally follow the contour of the anterior aspect of the
cervical vertebrae.
Based on the above discussion, how would you
interpret the lateral neck radiograph of the patient
discussed above?
View lateral neck.
c) Normally the air-soft tissue interface between the
prevertebral soft tissue and the air in the posterior
pharynx should be very sharp. Any inflammatory
process of the retropharyngeal space creates an
"indistinctness" and irregularity of this air-soft tissue
interface.
d) The contour of the prevertebral soft tissue should
normally follow the contour of the anterior aspect of the
cervical vertebrae.
Based on the above discussion, how would you
interpret the lateral neck radiograph of the patient
discussed above?
View lateral neck.
 Radiologist's interpretation: The lateral neck
radiograph reveals a moderate degree of soft tissue
swelling of the prevertebral/retropharyngeal soft tissues.
When the lateral neck radiograph suggests a
retropharyngeal infection, a CT scan of the neck should
be obtained to:
a) Delineate the extent of the infection (i.e., how far
down the pharynx, neck and chest does the infectious
process extend?).
b) Attempt to differentiate between a
retropharyngeal cellulitis/phlegmon versus a
retropharyngeal abscess.
Two characteristic findings that are suggestive of
an abscess are:
a) A rim of enhancement around a hypodense mass.
b) A convex appearance ("bulging-appearance") of
the surface of the hypodense mass. In contrast to this,
a phlegmon (pyogenic cellulitis) typically does not have
a rim of enhancement around the hypodense mass and
the surfaces of the phlegmon do not typically exhibit a
convex appearance.
A neck CT scan (with IV contrast) is obtained on the
patient discussed above. Based on the above
discussion, how would you interpret this patient's neck
CT scan?
View CT.
Radiologist's interpretation: The lateral neck
radiograph reveals a moderate degree of soft tissue
swelling of the prevertebral/retropharyngeal soft tissues.
When the lateral neck radiograph suggests a
retropharyngeal infection, a CT scan of the neck should
be obtained to:
a) Delineate the extent of the infection (i.e., how far
down the pharynx, neck and chest does the infectious
process extend?).
b) Attempt to differentiate between a
retropharyngeal cellulitis/phlegmon versus a
retropharyngeal abscess.
Two characteristic findings that are suggestive of
an abscess are:
a) A rim of enhancement around a hypodense mass.
b) A convex appearance ("bulging-appearance") of
the surface of the hypodense mass. In contrast to this,
a phlegmon (pyogenic cellulitis) typically does not have
a rim of enhancement around the hypodense mass and
the surfaces of the phlegmon do not typically exhibit a
convex appearance.
A neck CT scan (with IV contrast) is obtained on the
patient discussed above. Based on the above
discussion, how would you interpret this patient's neck
CT scan?
View CT.
 Radiologist's interpretation: There is a slight degree
of thickening of the prevertebral/retropharyngeal
soft-tissues. There is a plaque-like area of hypodensity
(arrow) anterior to the vertebral bodies and the longus
colli muscles which probably represents a fluid
collection in the retropharyngeal soft tissues without
definite abscess formation.
This case is most consistent with a retropharyngeal
phlegmon (pyogenic cellulitis) rather than a true
absence. There is no rim of enhancement (with
contrast) around the lesion and the soft tissues do not
bulge anteriorly in a convex fashion.
View abscess example.
Radiologist's interpretation: There is a slight degree
of thickening of the prevertebral/retropharyngeal
soft-tissues. There is a plaque-like area of hypodensity
(arrow) anterior to the vertebral bodies and the longus
colli muscles which probably represents a fluid
collection in the retropharyngeal soft tissues without
definite abscess formation.
This case is most consistent with a retropharyngeal
phlegmon (pyogenic cellulitis) rather than a true
absence. There is no rim of enhancement (with
contrast) around the lesion and the soft tissues do not
bulge anteriorly in a convex fashion.
View abscess example.
 This CT scan (with contrast) shows CT findings
more consistent with an abscess rather than a
phlegmon. Note the larger size, the rim of contrast
enhancement around the lesion and the anterior bulging
(convexity) of the prevertebral soft tissues. These
findings are suggestive of an abscess.
Discussion:
Retropharyngeal abscesses are the second most
common of the deep neck infections in children (second
only to peritonsillar abscesses which account for up to
50% of the deep neck infections in the pediatric
population).
The most common pathophysiologic etiology of a
retropharyngeal abscess is via suppurative adenitis of
the paramedian chains of lymphoid tissue (that drain
the nasopharynx, adenoids and posterior paranasal
sinuses) located in the retropharyngeal space. Thus,
otitis media and nasopharyngeal infections may lead to
suppuration of these paramedian chains of lymphoid
tissue and result in a retropharyngeal abscess.
Because this paramedian lymph tissue usually begins
to atrophy during the third to fourth year of life, it is no
surprise that the majority of retropharyngeal abscess
cases (50%) occur in children 6-12 months of age, with
96% of the cases occurring in children < 6 years of age.
Two other pathophysiologic etiologies of
retropharyngeal abscesses are via: 1) Direct
penetrating trauma to the retropharyngeal space (i.e., a
child who falls with a popsicle stick in his mouth and
sustains direct penetration of the posterior pharynx),
and 2) Anterior extension of a vertebral osteomyelitis
into the pre-vertebral soft tissue space.
A child with a retropharyngeal infection may present
with fever, sore throat, dysphagia and/or neck pain. If
the retropharyngeal infection is significant enough to
begin to compromise the patency of the child's posterior
pharynx, the patient may also present in a toxic fashion
with drooling and stridor (and thus mimicking the
presentation of a child with epiglottitis or croup). A child
with a retropharyngeal abscess may also present with
meningeal signs such as neck pain/stiffness secondary
to irritation of the paravertebral ligaments. Although
many textbooks comment on the fact that the posterior
pharynx of a child with a retropharyngeal abscess may
appear to be "bulging", in my personal experience this
physical examination finding has not been very obvious
in children with very early retropharyngeal infections
(i.e., cellulitis / phlegmon). Anterior deviation of the
uvula may also be present in a child with a
retropharyngeal infection. Examination of the
oropharynx should also be deferred if the child with a
possible retropharyngeal abscess presents in a
dramatic fashion with drooling and stridor.
Complications of a retropharyngeal abscess include:
1) Acute airway obstruction via obstruction of the
posterior pharynx.
2) Aspiration secondary to the child's inability to
handle his/her own oral secretions.
3) Rupture of the abscess into the pharynx resulting
in aspiration.
4) Extension of the abscess causing mediastinitis,
pneumonia or necrotizing fasciitis.
5) Sepsis
6) Dehydration secondary to the child's inability to
tolerate oral fluids.
The two most common organisms recovered from
retropharyngeal abscess cultures are Staphylococcus
aureus and Group A beta-hemolytic Streptococcus. A
child with a retropharyngeal cellulitis should be
hospitalized for intravenous antibiotics and observation
for potential airway compromise. If a retropharyngeal
abscess is diagnosed on the neck CT scan, the child
will also require surgical drainage of the abscess in
addition to intravenous antibiotics. Empiric antibiotic
regimens for a child with a retropharyngeal abscess
should cover for Staphylococcus aureus, Group A
beta-hemolytic Streptococcus and anaerobes (i.e.,
Bacteroides). Options include: oxacillin, first
generation cephalosporins, and/or clindamycin.
Consider the empiric use of vancomycin to cover the
possibility of methicillin resistant Staph aureus (MRSA).
Should this possibility materialize, sepsis may result
without adequate coverage.
Post-discussion quiz questions:
1) The majority of retropharyngeal abscess cases
occur in which age group?
a) < 1 year of age
b) 2 - 6 years of age
c) 7 - 10 years of age
d) > 12 years of age
2) List the three pathophysiologic mechanisms which
are responsible for producing a retropharyngeal
abscess:
a)
b)
c)
3) What are the two most common organisms that are
recovered from retropharyngeal abscess cultures?
a)
b)
4) The radiographic technique to optimally visualize the
prevertebral soft tissues on the lateral neck view is
during:
a) End-INSPiration with the patient's neck in the
flexed position.
b) End-EXPiration with the patient's neck in the
flexed position.
c) End-INSPiration with the patient's neck in the
extended position.
d) End-EXPiration with the patient's neck in the
flexed position.
5) List at least 3 potential complications of a
retropharyngeal abscess:
a)
b)
c)
References:
Abrunzo TJ, Santamaria JP. Peritonsillar Abscess
and Retropharyngeal Abscess. In: Strange GR, et al.
Pediatric Emergency Medicine: A Comprehensive
Study Guide. New York, McGraw-Hill; pp. 414-416,
1996.
Harris JH, et al. Radiographic Anatomy of the Neck.
In: The Radiology of Emergency Medicine (Third
Edition). Baltimore, Williams & Wilkins; pp. 133-138,
1993.
Sanatamaria JP, Abrunzo TJ. Peritonsillar Abscess
and Retropharyngeal Abscess. In: Barkin RA, et al.
Pediatric Emergency Medicine: Concepts and Clinical
Practice. St Louis, Mosby Year Book; pp. 679-681,
1992.
Swischuk LE. Retropharyngeal Abscess. In:
Emergency Imaging of the Acutely Ill or Injured Child
(Third Edition). Baltimore, Williams & Wilkins; pp.
171-175, 1994.
This CT scan (with contrast) shows CT findings
more consistent with an abscess rather than a
phlegmon. Note the larger size, the rim of contrast
enhancement around the lesion and the anterior bulging
(convexity) of the prevertebral soft tissues. These
findings are suggestive of an abscess.
Discussion:
Retropharyngeal abscesses are the second most
common of the deep neck infections in children (second
only to peritonsillar abscesses which account for up to
50% of the deep neck infections in the pediatric
population).
The most common pathophysiologic etiology of a
retropharyngeal abscess is via suppurative adenitis of
the paramedian chains of lymphoid tissue (that drain
the nasopharynx, adenoids and posterior paranasal
sinuses) located in the retropharyngeal space. Thus,
otitis media and nasopharyngeal infections may lead to
suppuration of these paramedian chains of lymphoid
tissue and result in a retropharyngeal abscess.
Because this paramedian lymph tissue usually begins
to atrophy during the third to fourth year of life, it is no
surprise that the majority of retropharyngeal abscess
cases (50%) occur in children 6-12 months of age, with
96% of the cases occurring in children < 6 years of age.
Two other pathophysiologic etiologies of
retropharyngeal abscesses are via: 1) Direct
penetrating trauma to the retropharyngeal space (i.e., a
child who falls with a popsicle stick in his mouth and
sustains direct penetration of the posterior pharynx),
and 2) Anterior extension of a vertebral osteomyelitis
into the pre-vertebral soft tissue space.
A child with a retropharyngeal infection may present
with fever, sore throat, dysphagia and/or neck pain. If
the retropharyngeal infection is significant enough to
begin to compromise the patency of the child's posterior
pharynx, the patient may also present in a toxic fashion
with drooling and stridor (and thus mimicking the
presentation of a child with epiglottitis or croup). A child
with a retropharyngeal abscess may also present with
meningeal signs such as neck pain/stiffness secondary
to irritation of the paravertebral ligaments. Although
many textbooks comment on the fact that the posterior
pharynx of a child with a retropharyngeal abscess may
appear to be "bulging", in my personal experience this
physical examination finding has not been very obvious
in children with very early retropharyngeal infections
(i.e., cellulitis / phlegmon). Anterior deviation of the
uvula may also be present in a child with a
retropharyngeal infection. Examination of the
oropharynx should also be deferred if the child with a
possible retropharyngeal abscess presents in a
dramatic fashion with drooling and stridor.
Complications of a retropharyngeal abscess include:
1) Acute airway obstruction via obstruction of the
posterior pharynx.
2) Aspiration secondary to the child's inability to
handle his/her own oral secretions.
3) Rupture of the abscess into the pharynx resulting
in aspiration.
4) Extension of the abscess causing mediastinitis,
pneumonia or necrotizing fasciitis.
5) Sepsis
6) Dehydration secondary to the child's inability to
tolerate oral fluids.
The two most common organisms recovered from
retropharyngeal abscess cultures are Staphylococcus
aureus and Group A beta-hemolytic Streptococcus. A
child with a retropharyngeal cellulitis should be
hospitalized for intravenous antibiotics and observation
for potential airway compromise. If a retropharyngeal
abscess is diagnosed on the neck CT scan, the child
will also require surgical drainage of the abscess in
addition to intravenous antibiotics. Empiric antibiotic
regimens for a child with a retropharyngeal abscess
should cover for Staphylococcus aureus, Group A
beta-hemolytic Streptococcus and anaerobes (i.e.,
Bacteroides). Options include: oxacillin, first
generation cephalosporins, and/or clindamycin.
Consider the empiric use of vancomycin to cover the
possibility of methicillin resistant Staph aureus (MRSA).
Should this possibility materialize, sepsis may result
without adequate coverage.
Post-discussion quiz questions:
1) The majority of retropharyngeal abscess cases
occur in which age group?
a) < 1 year of age
b) 2 - 6 years of age
c) 7 - 10 years of age
d) > 12 years of age
2) List the three pathophysiologic mechanisms which
are responsible for producing a retropharyngeal
abscess:
a)
b)
c)
3) What are the two most common organisms that are
recovered from retropharyngeal abscess cultures?
a)
b)
4) The radiographic technique to optimally visualize the
prevertebral soft tissues on the lateral neck view is
during:
a) End-INSPiration with the patient's neck in the
flexed position.
b) End-EXPiration with the patient's neck in the
flexed position.
c) End-INSPiration with the patient's neck in the
extended position.
d) End-EXPiration with the patient's neck in the
flexed position.
5) List at least 3 potential complications of a
retropharyngeal abscess:
a)
b)
c)
References:
Abrunzo TJ, Santamaria JP. Peritonsillar Abscess
and Retropharyngeal Abscess. In: Strange GR, et al.
Pediatric Emergency Medicine: A Comprehensive
Study Guide. New York, McGraw-Hill; pp. 414-416,
1996.
Harris JH, et al. Radiographic Anatomy of the Neck.
In: The Radiology of Emergency Medicine (Third
Edition). Baltimore, Williams & Wilkins; pp. 133-138,
1993.
Sanatamaria JP, Abrunzo TJ. Peritonsillar Abscess
and Retropharyngeal Abscess. In: Barkin RA, et al.
Pediatric Emergency Medicine: Concepts and Clinical
Practice. St Louis, Mosby Year Book; pp. 679-681,
1992.
Swischuk LE. Retropharyngeal Abscess. In:
Emergency Imaging of the Acutely Ill or Injured Child
(Third Edition). Baltimore, Williams & Wilkins; pp.
171-175, 1994.