Intracranial Hypertension and Brain Herniation Syndromes
Radiology Cases in Pediatric Emergency Medicine
Volume 5, Case 6
Loren G. Yamamoto, MD, MPH
Kapiolani Medical Center For Women And Children
University of Hawaii John A. Burns School of Medicine
This is a 5-year old female who is brought to the
emergency department at 8:00 a.m. because she was
poorly responsive when her mother awoke her in the
morning. This prompted her mother to drive her to the
E.D. There is a history of headache and vomiting
during the evening and night. There is no history of
trauma.
Exam: VS T36.7 (rectal), P92, R32, BP 137/97.
She is minimally responsive. Pupils equal and reactive.
There are no signs of external trauma.
Within minutes of arrival, she exhibits extensor
posturing. She is orally intubated using the rapid
sequence induction method with atropine, thiopental,
and vecuronium. She is hyperventilated. End-tidal
CO2 monitoring is used to keep her pCO2 in the 25
mmHg range. A loading dose of phenytoin is
administered.
An emergency CT scan is ordered.
View CT scan.
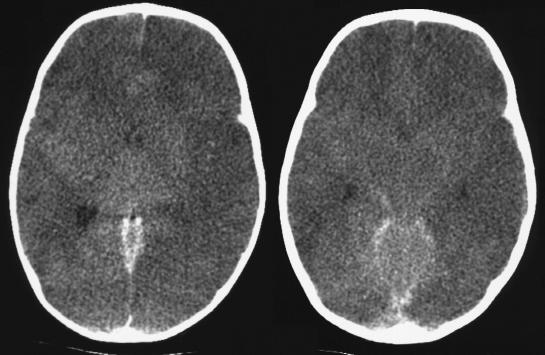
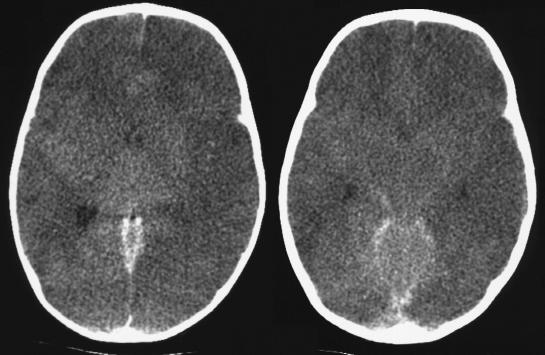
 There is obvious bilateral intraventricular
hemorrhage and ventricular dilatation. Clinically,
extensor posturing suggests the possibility of impending
herniation. She sustains episodes of bradycardia which
respond to doses of IV mannitol. A neurosurgeon
decompresses her ventricles immediately. She
recovers well without neurological deficits. Subsequent
studies demonstrate the presence of a choroid plexus
arteriovenous malformation. This is neurosurgically
ablated.
Discussion
Increases in intracranial pressure (ICP) compress
the brain within the rigid skull. This reduces cerebral
blood flow prompting reflex hypertension to maintain
cerebral perfusion. As intracranial pressure increases
further, the contents of the skull can no longer remain in
place. Focal increases in pressure, such as with
tumors and acute hemorrhages, result in focal
deviations in anatomy. While the term "herniation" is
used loosely when intracranial pressure increases,
there are specific herniation syndromes with different
mechanisms and outcomes. Identifying increases in
intracranial pressure by clinical and radiographic means
is important to intervene early to prevent herniation.
Clinical signs and symptoms of acute increased
intracranial pressure include, headache, vomiting, vision
distortion, diminished sensorium, pupillary dysfunction,
hypertension, bradycardia, flexor/extensor posturing,
etc. Papilledema may not be present if ICP increases
acutely.
When intracranial hypertension is suspected, an
immediate CT scan should be obtained to assess the
degree of ICP increase and to identify the cause of the
this.
The following areas should be assessed on CT
when attempting to determine the presence and
severity of intracranial hypertension. These are
discussed in more detail below.
1. Prominence of sulci/gyri.
2. Lateral ventricle size.
3. Grey/White matter distinction.
4. Suprasellar cistern.
5. Quadrigeminal cistern.
There are several brain herniation syndromes.
These are discussed in more detail below.
1. Uncal herniation.
2. Transtentorial herniation.
3. Tonsillar herniation.
4. Subfalcine herniation.
5. Superior vermian herniation.
CT signs of intracranial hypertension:
1. Prominence of sulci/gyri:
When intracranial pressure increases, this
compresses the cerebral cortex against the calvarium.
This attenuates the visibility of the sulci and gyri.
Additionally, the space between the cortex and the
calvarium is minimal when ICP increases.
View loss of sulci/gyri.
There is obvious bilateral intraventricular
hemorrhage and ventricular dilatation. Clinically,
extensor posturing suggests the possibility of impending
herniation. She sustains episodes of bradycardia which
respond to doses of IV mannitol. A neurosurgeon
decompresses her ventricles immediately. She
recovers well without neurological deficits. Subsequent
studies demonstrate the presence of a choroid plexus
arteriovenous malformation. This is neurosurgically
ablated.
Discussion
Increases in intracranial pressure (ICP) compress
the brain within the rigid skull. This reduces cerebral
blood flow prompting reflex hypertension to maintain
cerebral perfusion. As intracranial pressure increases
further, the contents of the skull can no longer remain in
place. Focal increases in pressure, such as with
tumors and acute hemorrhages, result in focal
deviations in anatomy. While the term "herniation" is
used loosely when intracranial pressure increases,
there are specific herniation syndromes with different
mechanisms and outcomes. Identifying increases in
intracranial pressure by clinical and radiographic means
is important to intervene early to prevent herniation.
Clinical signs and symptoms of acute increased
intracranial pressure include, headache, vomiting, vision
distortion, diminished sensorium, pupillary dysfunction,
hypertension, bradycardia, flexor/extensor posturing,
etc. Papilledema may not be present if ICP increases
acutely.
When intracranial hypertension is suspected, an
immediate CT scan should be obtained to assess the
degree of ICP increase and to identify the cause of the
this.
The following areas should be assessed on CT
when attempting to determine the presence and
severity of intracranial hypertension. These are
discussed in more detail below.
1. Prominence of sulci/gyri.
2. Lateral ventricle size.
3. Grey/White matter distinction.
4. Suprasellar cistern.
5. Quadrigeminal cistern.
There are several brain herniation syndromes.
These are discussed in more detail below.
1. Uncal herniation.
2. Transtentorial herniation.
3. Tonsillar herniation.
4. Subfalcine herniation.
5. Superior vermian herniation.
CT signs of intracranial hypertension:
1. Prominence of sulci/gyri:
When intracranial pressure increases, this
compresses the cerebral cortex against the calvarium.
This attenuates the visibility of the sulci and gyri.
Additionally, the space between the cortex and the
calvarium is minimal when ICP increases.
View loss of sulci/gyri.
 The image on the left is a high CT cut which should
show the sulci and gyri well. Due to increased ICP, the
cortex is compressed up against the calvarium losing
the distinctness of the sulci and gyri. The space
between the cortex and the calvarium is obliterated.
The sulci/gyri sign cannot be totally relied upon in
some instances. In cases of external hydrocephalus or
chronic (or subacute) subdural effusions, fluid collects
over the cortex. The fluid space between the cortex
and the calvarium appears to be increased and the
sulci/gyri may appear prominent.
View prominent sulci/gyri.
The image on the left is a high CT cut which should
show the sulci and gyri well. Due to increased ICP, the
cortex is compressed up against the calvarium losing
the distinctness of the sulci and gyri. The space
between the cortex and the calvarium is obliterated.
The sulci/gyri sign cannot be totally relied upon in
some instances. In cases of external hydrocephalus or
chronic (or subacute) subdural effusions, fluid collects
over the cortex. The fluid space between the cortex
and the calvarium appears to be increased and the
sulci/gyri may appear prominent.
View prominent sulci/gyri.
 Shown here is a focal extra-axial hematoma. Note
the prominent sulci and gyri despite intracranial
hemorrhage.
2. Lateral ventricle size:
In acute hydrocephalus, due to obstruction in the
outflow of CSF, the lateral ventricles will be enlarged.
Similarly, in acute intraventricular hemorrhage, the
lateral ventricles will be enlarged.
View dilated ventricles.
Shown here is a focal extra-axial hematoma. Note
the prominent sulci and gyri despite intracranial
hemorrhage.
2. Lateral ventricle size:
In acute hydrocephalus, due to obstruction in the
outflow of CSF, the lateral ventricles will be enlarged.
Similarly, in acute intraventricular hemorrhage, the
lateral ventricles will be enlarged.
View dilated ventricles.
 Shown here are bilateral dilated lateral ventricles
due to acute intraventricular hemorrhage.
In other causes of intracranial hypertension, the
lateral ventricles will be compressed (slit-like) or
obliterated due to increases in pressure in
compartments other than the lateral ventricles. This is
the case in generalized cerebral edema, subdural
hematoma, epidural hematoma, etc.
View compressed ventricles.
Shown here are bilateral dilated lateral ventricles
due to acute intraventricular hemorrhage.
In other causes of intracranial hypertension, the
lateral ventricles will be compressed (slit-like) or
obliterated due to increases in pressure in
compartments other than the lateral ventricles. This is
the case in generalized cerebral edema, subdural
hematoma, epidural hematoma, etc.
View compressed ventricles.
 Shown here are two cuts showing subarachnoid
hemorrhage. The ventricles are slit-like due to cerebral
edema and acute hemorrhage resulting in intracranial
hypertension.
3. Grey/White matter distinction:
This is mostly a sign of cerebral edema in
association with elevated ICP.
View good grey/white matter distinction.
Shown here are two cuts showing subarachnoid
hemorrhage. The ventricles are slit-like due to cerebral
edema and acute hemorrhage resulting in intracranial
hypertension.
3. Grey/White matter distinction:
This is mostly a sign of cerebral edema in
association with elevated ICP.
View good grey/white matter distinction.
 View poor grey/white matter distinction.
View poor grey/white matter distinction.
 4. Suprasellar cistern:
The suprasellar cistern is a fluid-filled space above
the sella turcica. It contains the circle of Willis and the
optic chiasm. On CT scan, it has a star-shaped
appearance. Anteriorly, the top point of the star is
formed by the interhemispheric fissure between the two
frontal lobes. The lateral border of the suprasellar
cistern is formed by the uncal portion of the temporal
lobes. The posterior border is formed by the pons in
lower cuts and the cerebral peduncles of the midbrain in
higher cuts. In lower cuts where the pons forms the
posterior border of the suprasellar cistern, the
suprasellar cistern takes on the shape of a 5-pointed
star. In cuts where the cerebral peduncles (which have
a central cleft) form the posterior border of the
suprasellar cistern, the suprasellar cistern takes on the
shape of a 6-pointed star.
View the midline anatomic diagram of the brain.
4. Suprasellar cistern:
The suprasellar cistern is a fluid-filled space above
the sella turcica. It contains the circle of Willis and the
optic chiasm. On CT scan, it has a star-shaped
appearance. Anteriorly, the top point of the star is
formed by the interhemispheric fissure between the two
frontal lobes. The lateral border of the suprasellar
cistern is formed by the uncal portion of the temporal
lobes. The posterior border is formed by the pons in
lower cuts and the cerebral peduncles of the midbrain in
higher cuts. In lower cuts where the pons forms the
posterior border of the suprasellar cistern, the
suprasellar cistern takes on the shape of a 5-pointed
star. In cuts where the cerebral peduncles (which have
a central cleft) form the posterior border of the
suprasellar cistern, the suprasellar cistern takes on the
shape of a 6-pointed star.
View the midline anatomic diagram of the brain.
 This is a midline sagittal cut of an MRI scan. Identify
the following structures:
S - suprasellar cistern
Po - pons
P - cerebral peduncles (midbrain)
M - medulla
C - quadrigeminal plate (superior and inferior colliculi)
V - fourth ventricle
Q - quadrigeminal cistern
Note that the fourth ventricle is connected to the
third ventricle by the cerebral aqueduct which is very
thin and may not be visible on CT.
View the anatomic diagram of the suprasellar cistern.
This is a midline sagittal cut of an MRI scan. Identify
the following structures:
S - suprasellar cistern
Po - pons
P - cerebral peduncles (midbrain)
M - medulla
C - quadrigeminal plate (superior and inferior colliculi)
V - fourth ventricle
Q - quadrigeminal cistern
Note that the fourth ventricle is connected to the
third ventricle by the cerebral aqueduct which is very
thin and may not be visible on CT.
View the anatomic diagram of the suprasellar cistern.
 The midline sagittal MRI scan shows the levels of
the axial diagrams. Note that the fourth ventricle is at
roughly the same level of the suprasellar cistern, but
depending on the angle of the axial cut, the fourth
ventricle may be seen in cuts above, below, or at the
same level as the suprasellar cistern. The suprasellar
cistern is seen in cuts 7 and 8.
In the lower cut (7), the suprasellar cistern (s) takes
on the shape of a five pointed star. The frontal lobes
(F) form the anterior border with the anterior
interhemispheric fissure between the frontal lobes
forming the apex of the star. The uncus (U) of the
temporal lobes forms the lateral borders. The pons
(Po) forms the posterior border. The fourth ventricle (V)
is also seen in this cut.
In the higher cut (8), the suprasellar cistern (s) takes
on the shape of a six pointed star. The only difference
higher up is that the posterior border is formed by the
cerebral peduncles (p) of the midbrain. The cleft
between the cerebral peduncles forms the sixth point of
the star. The inferior colliculi (c) can also be seen at
this level of the suprasellar cistern.
View CT scan of suprasellar cistern.
The midline sagittal MRI scan shows the levels of
the axial diagrams. Note that the fourth ventricle is at
roughly the same level of the suprasellar cistern, but
depending on the angle of the axial cut, the fourth
ventricle may be seen in cuts above, below, or at the
same level as the suprasellar cistern. The suprasellar
cistern is seen in cuts 7 and 8.
In the lower cut (7), the suprasellar cistern (s) takes
on the shape of a five pointed star. The frontal lobes
(F) form the anterior border with the anterior
interhemispheric fissure between the frontal lobes
forming the apex of the star. The uncus (U) of the
temporal lobes forms the lateral borders. The pons
(Po) forms the posterior border. The fourth ventricle (V)
is also seen in this cut.
In the higher cut (8), the suprasellar cistern (s) takes
on the shape of a six pointed star. The only difference
higher up is that the posterior border is formed by the
cerebral peduncles (p) of the midbrain. The cleft
between the cerebral peduncles forms the sixth point of
the star. The inferior colliculi (c) can also be seen at
this level of the suprasellar cistern.
View CT scan of suprasellar cistern.
 The left and center images show the suprasellar
cistern. Its anterior borders are formed by the frontal
lobes (F). Its lateral borders are formed by the uncus
(U) of the temporal lobes. The left image shows the
5-pointed star appearance of the suprasellar cistern
where the posterior border is formed by the pons (Po).
The black arrow points to the fourth ventricle. The
center image shows a higher cut where the suprasellar
cistern has a 6-pointed star appearance since the
posterior border is formed by the cerebral peduncles
(P) which have a central cleft.
When ICP increases, the suprasellar cistern space
is compressed. The space may still be visible;
however, with severe intracranial hypertension, the
cistern is obliterated due to encroachment of brain
tissue that normally forms the borders of the suprasellar
cistern. Depending on the cause of the intracranial
hypertension, the suprasellar cistern may be totally
obliterated in global or severe ICP increase. In focal
lesions, brain tissue may encroach into only one part of
the suprasellar cistern. In early unilateral uncal
herniation, the uncus of the temporal lobe (lateral
border of the suprasellar cistern) will protrude into the
suprasellar cistern.
5. Quadrigeminal cistern:
Also known as the quadrigeminal plate cistern, this
fluid filled space is located cephalad to the fourth
ventricle.
View the anatomic diagram of the quadrigeminal
cistern.
The left and center images show the suprasellar
cistern. Its anterior borders are formed by the frontal
lobes (F). Its lateral borders are formed by the uncus
(U) of the temporal lobes. The left image shows the
5-pointed star appearance of the suprasellar cistern
where the posterior border is formed by the pons (Po).
The black arrow points to the fourth ventricle. The
center image shows a higher cut where the suprasellar
cistern has a 6-pointed star appearance since the
posterior border is formed by the cerebral peduncles
(P) which have a central cleft.
When ICP increases, the suprasellar cistern space
is compressed. The space may still be visible;
however, with severe intracranial hypertension, the
cistern is obliterated due to encroachment of brain
tissue that normally forms the borders of the suprasellar
cistern. Depending on the cause of the intracranial
hypertension, the suprasellar cistern may be totally
obliterated in global or severe ICP increase. In focal
lesions, brain tissue may encroach into only one part of
the suprasellar cistern. In early unilateral uncal
herniation, the uncus of the temporal lobe (lateral
border of the suprasellar cistern) will protrude into the
suprasellar cistern.
5. Quadrigeminal cistern:
Also known as the quadrigeminal plate cistern, this
fluid filled space is located cephalad to the fourth
ventricle.
View the anatomic diagram of the quadrigeminal
cistern.
 The midline sagittal MRI scan shows the levels of
the axial diagrams. The quadrigeminal cistern is
located above (anterior to) the "Q" in the highest cut
shown (number 9). The anterior border of the
quadrigeminal cistern is formed by the superior colliculi
(c). Image 8 (lower cut) also shows the quadrigeminal
cistern. In this case, its anterior border is formed by the
inferior colliculi (c). This gives the anterior border of the
quadrigeminal cistern the appearance of a "baby's
bottom". The quadrigeminal plate is comprised of the
superior and inferior colliculi. The quadrigeminal cistern
is posterior to this quadrigeminal plate, thus its anterior
border may be formed by the inferior or superior
colliculi.
View CT scan of quadrigeminal cistern.
The midline sagittal MRI scan shows the levels of
the axial diagrams. The quadrigeminal cistern is
located above (anterior to) the "Q" in the highest cut
shown (number 9). The anterior border of the
quadrigeminal cistern is formed by the superior colliculi
(c). Image 8 (lower cut) also shows the quadrigeminal
cistern. In this case, its anterior border is formed by the
inferior colliculi (c). This gives the anterior border of the
quadrigeminal cistern the appearance of a "baby's
bottom". The quadrigeminal plate is comprised of the
superior and inferior colliculi. The quadrigeminal cistern
is posterior to this quadrigeminal plate, thus its anterior
border may be formed by the inferior or superior
colliculi.
View CT scan of quadrigeminal cistern.
 The right image shows the quadrigeminal cistern
(black arrow). Note the "baby's bottom" appearance of
its anterior border. When ICP is increased, the
quadrigeminal cistern space is compressed or
obliterated.
Identify the suprasellar and quadrigeminal cisterns in
the following examples.
View moderately increased ICP.
The right image shows the quadrigeminal cistern
(black arrow). Note the "baby's bottom" appearance of
its anterior border. When ICP is increased, the
quadrigeminal cistern space is compressed or
obliterated.
Identify the suprasellar and quadrigeminal cisterns in
the following examples.
View moderately increased ICP.
 The suprasellar cistern is slightly smaller than its
normal size (the right uncus is pushing into the
suprasellar cistern) and the quadrigeminal cistern is
compressed. An epidural hematoma is noted.
View severe ICP increase.
The suprasellar cistern is slightly smaller than its
normal size (the right uncus is pushing into the
suprasellar cistern) and the quadrigeminal cistern is
compressed. An epidural hematoma is noted.
View severe ICP increase.
 The suprasellar cistern (left image) is tissue-filled,
indicating the presence of brain tissue herniating into
this space. The quadrigeminal cistern is very
compressed and pushed posteriorly (center image).
The suprasellar cistern is located just above the base of
the skull (above the sella). It should be visible in the
cuts near the base of the brain. If it is not visible, it
suggests that the suprasellar cistern is obliterated.
Similarly, the quadrigeminal cistern should be located in
the cut above the suprasellar cistern. A subdural
hematoma is noted with a midline shift.
Brain Herniation Syndromes:
1. Uncal herniation:
When mass effects within or adjacent to the
temporal lobe occur, the medial portion of the temporal
lobe (uncus) is forced medially and downward over the
tentorium. There is ipsilateral pupillary dilation. The
uncus is pushed medially into the suprasellar cistern.
View uncal herniation.
The suprasellar cistern (left image) is tissue-filled,
indicating the presence of brain tissue herniating into
this space. The quadrigeminal cistern is very
compressed and pushed posteriorly (center image).
The suprasellar cistern is located just above the base of
the skull (above the sella). It should be visible in the
cuts near the base of the brain. If it is not visible, it
suggests that the suprasellar cistern is obliterated.
Similarly, the quadrigeminal cistern should be located in
the cut above the suprasellar cistern. A subdural
hematoma is noted with a midline shift.
Brain Herniation Syndromes:
1. Uncal herniation:
When mass effects within or adjacent to the
temporal lobe occur, the medial portion of the temporal
lobe (uncus) is forced medially and downward over the
tentorium. There is ipsilateral pupillary dilation. The
uncus is pushed medially into the suprasellar cistern.
View uncal herniation.
 There is bilateral uncal herniation. The suprasellar
cistern is obliterated.
View early uncal herniation.
There is bilateral uncal herniation. The suprasellar
cistern is obliterated.
View early uncal herniation.
 The right uncus is pushing into the suprasellar
cistern; early right uncal herniation.
2. Transtentorial herniation:
It should be noted that this term is somewhat vague.
It is used rather loosely and it may sometimes be used
similarly to the terms temporal lobe herniation and uncal
herniation. The uncus may herniate over the tentorium
as described above. Supratentorial lesions on one side
may initially result in uncal herniation. As ICP increases
further, bilateral temporal lobe herniation occurs
transtentorially. Early unilateral uncal herniation is
more accurately called uncal herniation. The terms
cranial-caudal transtentorial herniation, rostro-caudal
transtentorial herniation, or central transtentorial
herniation more accurately describe what is generally
meant by "transtentorial herniation". Thus, uncal
herniation is described separately above.
In transtentorial herniation the medial portions of the
temporal lobes (uncus) and the brainstem herniate
downward from supratentorial to the infratentorial
compartment. The clinical signs include headache,
decreasing level of consciousness and ipsilateral fixed
dilated pupil (from compression of the third cranial
nerve on the ipsilateral side). As herniation worsens,
decerebrate (extensor) posturing, contralateral (ie.,
bilateral) pupillary dilation and Cushing's triad occur.
Cushing's triad includes alteration in respiration,
bradycardia, and systemic hypertension. It is rare to
have all three present in children. Often there is just
bradycardia alone. Children tolerate brainstem
compression produced by herniation better than adults.
Immediate early intervention can result in recovery.
Intervention at the stage of unilateral pupillary
dysfunction is likely to have a better prognosis
than intervention at the stage of bilateral pupillary
dysfunction, decerebrate posturing and bradycardia.
CT scan shows obliteration of the suprasellar and
quadrigeminal cisterns. Later findings include infarcts
and brainstem hemorrhage.
View transtentorial herniation.
The right uncus is pushing into the suprasellar
cistern; early right uncal herniation.
2. Transtentorial herniation:
It should be noted that this term is somewhat vague.
It is used rather loosely and it may sometimes be used
similarly to the terms temporal lobe herniation and uncal
herniation. The uncus may herniate over the tentorium
as described above. Supratentorial lesions on one side
may initially result in uncal herniation. As ICP increases
further, bilateral temporal lobe herniation occurs
transtentorially. Early unilateral uncal herniation is
more accurately called uncal herniation. The terms
cranial-caudal transtentorial herniation, rostro-caudal
transtentorial herniation, or central transtentorial
herniation more accurately describe what is generally
meant by "transtentorial herniation". Thus, uncal
herniation is described separately above.
In transtentorial herniation the medial portions of the
temporal lobes (uncus) and the brainstem herniate
downward from supratentorial to the infratentorial
compartment. The clinical signs include headache,
decreasing level of consciousness and ipsilateral fixed
dilated pupil (from compression of the third cranial
nerve on the ipsilateral side). As herniation worsens,
decerebrate (extensor) posturing, contralateral (ie.,
bilateral) pupillary dilation and Cushing's triad occur.
Cushing's triad includes alteration in respiration,
bradycardia, and systemic hypertension. It is rare to
have all three present in children. Often there is just
bradycardia alone. Children tolerate brainstem
compression produced by herniation better than adults.
Immediate early intervention can result in recovery.
Intervention at the stage of unilateral pupillary
dysfunction is likely to have a better prognosis
than intervention at the stage of bilateral pupillary
dysfunction, decerebrate posturing and bradycardia.
CT scan shows obliteration of the suprasellar and
quadrigeminal cisterns. Later findings include infarcts
and brainstem hemorrhage.
View transtentorial herniation.
 The suprasellar cistern (left image) is obliterated.
The quadrigeminal cistern is very compressed and
pushed posteriorly (center image). A subdural
hematoma with a midline shift is noted. There is central
transtentorial and subfalcine herniation.
3. Tonsillar herniation:
In tonsillar herniation (rare), a mass effect in the
posterior fossa causes the cerebellar tonsils to
herniate inferiorly through the foramen magnum
compressing the medulla and upper cervical spinal
cord. Conscious patients complain of neck pain and
vomiting. They may have nystagmus, pupillary
dilatation, bradycardia, hypertension and respiratory
depression. Early tonsillar herniation is difficult to
recognize in an unconscious patient. It may not be
evident on CT scan since axial views cannot see the
pathology well. It is best seen on sagittal MRI.
Clinically changes in vital signs may be the only clinical
clue in an unconscious patient.
4. Subfalcine herniation (cingulate herniation):
A unilateral supratentorial mass or hemorrhage
results in a midline shift. If the pressure pushing the
brain to one side is great enough, one of the
hemispheres is pushed under the falx (subfalcine). This
may compress the anterior cerebral artery. There is
ipsilateral lateral ventricle compression and
contralateral lateral ventricle dilation (due to obstruction
of the foramen of Monroe).
View subfalcine herniation.
The suprasellar cistern (left image) is obliterated.
The quadrigeminal cistern is very compressed and
pushed posteriorly (center image). A subdural
hematoma with a midline shift is noted. There is central
transtentorial and subfalcine herniation.
3. Tonsillar herniation:
In tonsillar herniation (rare), a mass effect in the
posterior fossa causes the cerebellar tonsils to
herniate inferiorly through the foramen magnum
compressing the medulla and upper cervical spinal
cord. Conscious patients complain of neck pain and
vomiting. They may have nystagmus, pupillary
dilatation, bradycardia, hypertension and respiratory
depression. Early tonsillar herniation is difficult to
recognize in an unconscious patient. It may not be
evident on CT scan since axial views cannot see the
pathology well. It is best seen on sagittal MRI.
Clinically changes in vital signs may be the only clinical
clue in an unconscious patient.
4. Subfalcine herniation (cingulate herniation):
A unilateral supratentorial mass or hemorrhage
results in a midline shift. If the pressure pushing the
brain to one side is great enough, one of the
hemispheres is pushed under the falx (subfalcine). This
may compress the anterior cerebral artery. There is
ipsilateral lateral ventricle compression and
contralateral lateral ventricle dilation (due to obstruction
of the foramen of Monroe).
View subfalcine herniation.
 The suprasellar cistern (left image) is obliterated.
The quadrigeminal cistern is very compressed and
pushed posteriorly (center image). A subdural
hematoma with a midline shift is noted. There is central
transtentorial and subfalcine herniation.
5. Superior vermian herniation:
Also called ascending transtentorial herniation, this
involves upward herniation of the vermis and cerebellar
hemispheres through the tentorial incisura due to a
mass effect in the posterior fossa. There is effacement
of the quadrigeminal cistern. There is hydrocephalus
due to compression of the aqueduct of Sylvius.
References
Grossman RI, Yousem DM. Head Trauma. In:
Grossman RI, Yousem DM. Neuroradiology - The
Requisites. Mosby, St. Louis, 1994, pp. 149-169.
Bruce DA. Head Trauma. In: Fleisher GR, Ludwig
S (eds). Textbook of Pediatric Emergency Medicine,
3rd ed. Williams & Wilkins, Philadelphia, 1993. pp.
1102-1119.
Kirkwood RJ. Head Trauma. In: Kirkwood JR.
Essentials of Neuroimaging, second edition. Churchill
Livingstone, New York, 1995, pp. 339-359.
Truwit CL, Lempert TE. High Resolution Atlas of
Cranial Neuroanatomy. Williams & Wilkins, Baltimore,
1994.
Willing SJ. General Manifestations of Intracranial
Diseases. In: Willing SJ. Atlas of Neuroradiology.
W.B Saunders, Philadelphia, 1995, pp. 1-40.
Castillo M, Harris JH. Skull and Brain. In: Harris
JH, Harris WH, Novelline RA (eds). The Radiology of
Emergency Medicine. Williams & Wilkins, Baltimore,
1993, pp. 1-35.
The suprasellar cistern (left image) is obliterated.
The quadrigeminal cistern is very compressed and
pushed posteriorly (center image). A subdural
hematoma with a midline shift is noted. There is central
transtentorial and subfalcine herniation.
5. Superior vermian herniation:
Also called ascending transtentorial herniation, this
involves upward herniation of the vermis and cerebellar
hemispheres through the tentorial incisura due to a
mass effect in the posterior fossa. There is effacement
of the quadrigeminal cistern. There is hydrocephalus
due to compression of the aqueduct of Sylvius.
References
Grossman RI, Yousem DM. Head Trauma. In:
Grossman RI, Yousem DM. Neuroradiology - The
Requisites. Mosby, St. Louis, 1994, pp. 149-169.
Bruce DA. Head Trauma. In: Fleisher GR, Ludwig
S (eds). Textbook of Pediatric Emergency Medicine,
3rd ed. Williams & Wilkins, Philadelphia, 1993. pp.
1102-1119.
Kirkwood RJ. Head Trauma. In: Kirkwood JR.
Essentials of Neuroimaging, second edition. Churchill
Livingstone, New York, 1995, pp. 339-359.
Truwit CL, Lempert TE. High Resolution Atlas of
Cranial Neuroanatomy. Williams & Wilkins, Baltimore,
1994.
Willing SJ. General Manifestations of Intracranial
Diseases. In: Willing SJ. Atlas of Neuroradiology.
W.B Saunders, Philadelphia, 1995, pp. 1-40.
Castillo M, Harris JH. Skull and Brain. In: Harris
JH, Harris WH, Novelline RA (eds). The Radiology of
Emergency Medicine. Williams & Wilkins, Baltimore,
1993, pp. 1-35.
Return to Radiology Cases In Ped Emerg Med Case Selection Page
Return to Univ. Hawaii Dept. Pediatrics Home Page
 There is obvious bilateral intraventricular
hemorrhage and ventricular dilatation. Clinically,
extensor posturing suggests the possibility of impending
herniation. She sustains episodes of bradycardia which
respond to doses of IV mannitol. A neurosurgeon
decompresses her ventricles immediately. She
recovers well without neurological deficits. Subsequent
studies demonstrate the presence of a choroid plexus
arteriovenous malformation. This is neurosurgically
ablated.
Discussion
Increases in intracranial pressure (ICP) compress
the brain within the rigid skull. This reduces cerebral
blood flow prompting reflex hypertension to maintain
cerebral perfusion. As intracranial pressure increases
further, the contents of the skull can no longer remain in
place. Focal increases in pressure, such as with
tumors and acute hemorrhages, result in focal
deviations in anatomy. While the term "herniation" is
used loosely when intracranial pressure increases,
there are specific herniation syndromes with different
mechanisms and outcomes. Identifying increases in
intracranial pressure by clinical and radiographic means
is important to intervene early to prevent herniation.
Clinical signs and symptoms of acute increased
intracranial pressure include, headache, vomiting, vision
distortion, diminished sensorium, pupillary dysfunction,
hypertension, bradycardia, flexor/extensor posturing,
etc. Papilledema may not be present if ICP increases
acutely.
When intracranial hypertension is suspected, an
immediate CT scan should be obtained to assess the
degree of ICP increase and to identify the cause of the
this.
The following areas should be assessed on CT
when attempting to determine the presence and
severity of intracranial hypertension. These are
discussed in more detail below.
1. Prominence of sulci/gyri.
2. Lateral ventricle size.
3. Grey/White matter distinction.
4. Suprasellar cistern.
5. Quadrigeminal cistern.
There are several brain herniation syndromes.
These are discussed in more detail below.
1. Uncal herniation.
2. Transtentorial herniation.
3. Tonsillar herniation.
4. Subfalcine herniation.
5. Superior vermian herniation.
CT signs of intracranial hypertension:
1. Prominence of sulci/gyri:
When intracranial pressure increases, this
compresses the cerebral cortex against the calvarium.
This attenuates the visibility of the sulci and gyri.
Additionally, the space between the cortex and the
calvarium is minimal when ICP increases.
View loss of sulci/gyri.
There is obvious bilateral intraventricular
hemorrhage and ventricular dilatation. Clinically,
extensor posturing suggests the possibility of impending
herniation. She sustains episodes of bradycardia which
respond to doses of IV mannitol. A neurosurgeon
decompresses her ventricles immediately. She
recovers well without neurological deficits. Subsequent
studies demonstrate the presence of a choroid plexus
arteriovenous malformation. This is neurosurgically
ablated.
Discussion
Increases in intracranial pressure (ICP) compress
the brain within the rigid skull. This reduces cerebral
blood flow prompting reflex hypertension to maintain
cerebral perfusion. As intracranial pressure increases
further, the contents of the skull can no longer remain in
place. Focal increases in pressure, such as with
tumors and acute hemorrhages, result in focal
deviations in anatomy. While the term "herniation" is
used loosely when intracranial pressure increases,
there are specific herniation syndromes with different
mechanisms and outcomes. Identifying increases in
intracranial pressure by clinical and radiographic means
is important to intervene early to prevent herniation.
Clinical signs and symptoms of acute increased
intracranial pressure include, headache, vomiting, vision
distortion, diminished sensorium, pupillary dysfunction,
hypertension, bradycardia, flexor/extensor posturing,
etc. Papilledema may not be present if ICP increases
acutely.
When intracranial hypertension is suspected, an
immediate CT scan should be obtained to assess the
degree of ICP increase and to identify the cause of the
this.
The following areas should be assessed on CT
when attempting to determine the presence and
severity of intracranial hypertension. These are
discussed in more detail below.
1. Prominence of sulci/gyri.
2. Lateral ventricle size.
3. Grey/White matter distinction.
4. Suprasellar cistern.
5. Quadrigeminal cistern.
There are several brain herniation syndromes.
These are discussed in more detail below.
1. Uncal herniation.
2. Transtentorial herniation.
3. Tonsillar herniation.
4. Subfalcine herniation.
5. Superior vermian herniation.
CT signs of intracranial hypertension:
1. Prominence of sulci/gyri:
When intracranial pressure increases, this
compresses the cerebral cortex against the calvarium.
This attenuates the visibility of the sulci and gyri.
Additionally, the space between the cortex and the
calvarium is minimal when ICP increases.
View loss of sulci/gyri.
 The image on the left is a high CT cut which should
show the sulci and gyri well. Due to increased ICP, the
cortex is compressed up against the calvarium losing
the distinctness of the sulci and gyri. The space
between the cortex and the calvarium is obliterated.
The sulci/gyri sign cannot be totally relied upon in
some instances. In cases of external hydrocephalus or
chronic (or subacute) subdural effusions, fluid collects
over the cortex. The fluid space between the cortex
and the calvarium appears to be increased and the
sulci/gyri may appear prominent.
View prominent sulci/gyri.
The image on the left is a high CT cut which should
show the sulci and gyri well. Due to increased ICP, the
cortex is compressed up against the calvarium losing
the distinctness of the sulci and gyri. The space
between the cortex and the calvarium is obliterated.
The sulci/gyri sign cannot be totally relied upon in
some instances. In cases of external hydrocephalus or
chronic (or subacute) subdural effusions, fluid collects
over the cortex. The fluid space between the cortex
and the calvarium appears to be increased and the
sulci/gyri may appear prominent.
View prominent sulci/gyri.
 Shown here is a focal extra-axial hematoma. Note
the prominent sulci and gyri despite intracranial
hemorrhage.
2. Lateral ventricle size:
In acute hydrocephalus, due to obstruction in the
outflow of CSF, the lateral ventricles will be enlarged.
Similarly, in acute intraventricular hemorrhage, the
lateral ventricles will be enlarged.
View dilated ventricles.
Shown here is a focal extra-axial hematoma. Note
the prominent sulci and gyri despite intracranial
hemorrhage.
2. Lateral ventricle size:
In acute hydrocephalus, due to obstruction in the
outflow of CSF, the lateral ventricles will be enlarged.
Similarly, in acute intraventricular hemorrhage, the
lateral ventricles will be enlarged.
View dilated ventricles.
 Shown here are bilateral dilated lateral ventricles
due to acute intraventricular hemorrhage.
In other causes of intracranial hypertension, the
lateral ventricles will be compressed (slit-like) or
obliterated due to increases in pressure in
compartments other than the lateral ventricles. This is
the case in generalized cerebral edema, subdural
hematoma, epidural hematoma, etc.
View compressed ventricles.
Shown here are bilateral dilated lateral ventricles
due to acute intraventricular hemorrhage.
In other causes of intracranial hypertension, the
lateral ventricles will be compressed (slit-like) or
obliterated due to increases in pressure in
compartments other than the lateral ventricles. This is
the case in generalized cerebral edema, subdural
hematoma, epidural hematoma, etc.
View compressed ventricles.
 Shown here are two cuts showing subarachnoid
hemorrhage. The ventricles are slit-like due to cerebral
edema and acute hemorrhage resulting in intracranial
hypertension.
3. Grey/White matter distinction:
This is mostly a sign of cerebral edema in
association with elevated ICP.
View good grey/white matter distinction.
Shown here are two cuts showing subarachnoid
hemorrhage. The ventricles are slit-like due to cerebral
edema and acute hemorrhage resulting in intracranial
hypertension.
3. Grey/White matter distinction:
This is mostly a sign of cerebral edema in
association with elevated ICP.
View good grey/white matter distinction.
 View poor grey/white matter distinction.
View poor grey/white matter distinction.
 4. Suprasellar cistern:
The suprasellar cistern is a fluid-filled space above
the sella turcica. It contains the circle of Willis and the
optic chiasm. On CT scan, it has a star-shaped
appearance. Anteriorly, the top point of the star is
formed by the interhemispheric fissure between the two
frontal lobes. The lateral border of the suprasellar
cistern is formed by the uncal portion of the temporal
lobes. The posterior border is formed by the pons in
lower cuts and the cerebral peduncles of the midbrain in
higher cuts. In lower cuts where the pons forms the
posterior border of the suprasellar cistern, the
suprasellar cistern takes on the shape of a 5-pointed
star. In cuts where the cerebral peduncles (which have
a central cleft) form the posterior border of the
suprasellar cistern, the suprasellar cistern takes on the
shape of a 6-pointed star.
View the midline anatomic diagram of the brain.
4. Suprasellar cistern:
The suprasellar cistern is a fluid-filled space above
the sella turcica. It contains the circle of Willis and the
optic chiasm. On CT scan, it has a star-shaped
appearance. Anteriorly, the top point of the star is
formed by the interhemispheric fissure between the two
frontal lobes. The lateral border of the suprasellar
cistern is formed by the uncal portion of the temporal
lobes. The posterior border is formed by the pons in
lower cuts and the cerebral peduncles of the midbrain in
higher cuts. In lower cuts where the pons forms the
posterior border of the suprasellar cistern, the
suprasellar cistern takes on the shape of a 5-pointed
star. In cuts where the cerebral peduncles (which have
a central cleft) form the posterior border of the
suprasellar cistern, the suprasellar cistern takes on the
shape of a 6-pointed star.
View the midline anatomic diagram of the brain.
 This is a midline sagittal cut of an MRI scan. Identify
the following structures:
S - suprasellar cistern
Po - pons
P - cerebral peduncles (midbrain)
M - medulla
C - quadrigeminal plate (superior and inferior colliculi)
V - fourth ventricle
Q - quadrigeminal cistern
Note that the fourth ventricle is connected to the
third ventricle by the cerebral aqueduct which is very
thin and may not be visible on CT.
View the anatomic diagram of the suprasellar cistern.
This is a midline sagittal cut of an MRI scan. Identify
the following structures:
S - suprasellar cistern
Po - pons
P - cerebral peduncles (midbrain)
M - medulla
C - quadrigeminal plate (superior and inferior colliculi)
V - fourth ventricle
Q - quadrigeminal cistern
Note that the fourth ventricle is connected to the
third ventricle by the cerebral aqueduct which is very
thin and may not be visible on CT.
View the anatomic diagram of the suprasellar cistern.
 The midline sagittal MRI scan shows the levels of
the axial diagrams. Note that the fourth ventricle is at
roughly the same level of the suprasellar cistern, but
depending on the angle of the axial cut, the fourth
ventricle may be seen in cuts above, below, or at the
same level as the suprasellar cistern. The suprasellar
cistern is seen in cuts 7 and 8.
In the lower cut (7), the suprasellar cistern (s) takes
on the shape of a five pointed star. The frontal lobes
(F) form the anterior border with the anterior
interhemispheric fissure between the frontal lobes
forming the apex of the star. The uncus (U) of the
temporal lobes forms the lateral borders. The pons
(Po) forms the posterior border. The fourth ventricle (V)
is also seen in this cut.
In the higher cut (8), the suprasellar cistern (s) takes
on the shape of a six pointed star. The only difference
higher up is that the posterior border is formed by the
cerebral peduncles (p) of the midbrain. The cleft
between the cerebral peduncles forms the sixth point of
the star. The inferior colliculi (c) can also be seen at
this level of the suprasellar cistern.
View CT scan of suprasellar cistern.
The midline sagittal MRI scan shows the levels of
the axial diagrams. Note that the fourth ventricle is at
roughly the same level of the suprasellar cistern, but
depending on the angle of the axial cut, the fourth
ventricle may be seen in cuts above, below, or at the
same level as the suprasellar cistern. The suprasellar
cistern is seen in cuts 7 and 8.
In the lower cut (7), the suprasellar cistern (s) takes
on the shape of a five pointed star. The frontal lobes
(F) form the anterior border with the anterior
interhemispheric fissure between the frontal lobes
forming the apex of the star. The uncus (U) of the
temporal lobes forms the lateral borders. The pons
(Po) forms the posterior border. The fourth ventricle (V)
is also seen in this cut.
In the higher cut (8), the suprasellar cistern (s) takes
on the shape of a six pointed star. The only difference
higher up is that the posterior border is formed by the
cerebral peduncles (p) of the midbrain. The cleft
between the cerebral peduncles forms the sixth point of
the star. The inferior colliculi (c) can also be seen at
this level of the suprasellar cistern.
View CT scan of suprasellar cistern.
 The left and center images show the suprasellar
cistern. Its anterior borders are formed by the frontal
lobes (F). Its lateral borders are formed by the uncus
(U) of the temporal lobes. The left image shows the
5-pointed star appearance of the suprasellar cistern
where the posterior border is formed by the pons (Po).
The black arrow points to the fourth ventricle. The
center image shows a higher cut where the suprasellar
cistern has a 6-pointed star appearance since the
posterior border is formed by the cerebral peduncles
(P) which have a central cleft.
When ICP increases, the suprasellar cistern space
is compressed. The space may still be visible;
however, with severe intracranial hypertension, the
cistern is obliterated due to encroachment of brain
tissue that normally forms the borders of the suprasellar
cistern. Depending on the cause of the intracranial
hypertension, the suprasellar cistern may be totally
obliterated in global or severe ICP increase. In focal
lesions, brain tissue may encroach into only one part of
the suprasellar cistern. In early unilateral uncal
herniation, the uncus of the temporal lobe (lateral
border of the suprasellar cistern) will protrude into the
suprasellar cistern.
5. Quadrigeminal cistern:
Also known as the quadrigeminal plate cistern, this
fluid filled space is located cephalad to the fourth
ventricle.
View the anatomic diagram of the quadrigeminal
cistern.
The left and center images show the suprasellar
cistern. Its anterior borders are formed by the frontal
lobes (F). Its lateral borders are formed by the uncus
(U) of the temporal lobes. The left image shows the
5-pointed star appearance of the suprasellar cistern
where the posterior border is formed by the pons (Po).
The black arrow points to the fourth ventricle. The
center image shows a higher cut where the suprasellar
cistern has a 6-pointed star appearance since the
posterior border is formed by the cerebral peduncles
(P) which have a central cleft.
When ICP increases, the suprasellar cistern space
is compressed. The space may still be visible;
however, with severe intracranial hypertension, the
cistern is obliterated due to encroachment of brain
tissue that normally forms the borders of the suprasellar
cistern. Depending on the cause of the intracranial
hypertension, the suprasellar cistern may be totally
obliterated in global or severe ICP increase. In focal
lesions, brain tissue may encroach into only one part of
the suprasellar cistern. In early unilateral uncal
herniation, the uncus of the temporal lobe (lateral
border of the suprasellar cistern) will protrude into the
suprasellar cistern.
5. Quadrigeminal cistern:
Also known as the quadrigeminal plate cistern, this
fluid filled space is located cephalad to the fourth
ventricle.
View the anatomic diagram of the quadrigeminal
cistern.
 The midline sagittal MRI scan shows the levels of
the axial diagrams. The quadrigeminal cistern is
located above (anterior to) the "Q" in the highest cut
shown (number 9). The anterior border of the
quadrigeminal cistern is formed by the superior colliculi
(c). Image 8 (lower cut) also shows the quadrigeminal
cistern. In this case, its anterior border is formed by the
inferior colliculi (c). This gives the anterior border of the
quadrigeminal cistern the appearance of a "baby's
bottom". The quadrigeminal plate is comprised of the
superior and inferior colliculi. The quadrigeminal cistern
is posterior to this quadrigeminal plate, thus its anterior
border may be formed by the inferior or superior
colliculi.
View CT scan of quadrigeminal cistern.
The midline sagittal MRI scan shows the levels of
the axial diagrams. The quadrigeminal cistern is
located above (anterior to) the "Q" in the highest cut
shown (number 9). The anterior border of the
quadrigeminal cistern is formed by the superior colliculi
(c). Image 8 (lower cut) also shows the quadrigeminal
cistern. In this case, its anterior border is formed by the
inferior colliculi (c). This gives the anterior border of the
quadrigeminal cistern the appearance of a "baby's
bottom". The quadrigeminal plate is comprised of the
superior and inferior colliculi. The quadrigeminal cistern
is posterior to this quadrigeminal plate, thus its anterior
border may be formed by the inferior or superior
colliculi.
View CT scan of quadrigeminal cistern.
 The right image shows the quadrigeminal cistern
(black arrow). Note the "baby's bottom" appearance of
its anterior border. When ICP is increased, the
quadrigeminal cistern space is compressed or
obliterated.
Identify the suprasellar and quadrigeminal cisterns in
the following examples.
View moderately increased ICP.
The right image shows the quadrigeminal cistern
(black arrow). Note the "baby's bottom" appearance of
its anterior border. When ICP is increased, the
quadrigeminal cistern space is compressed or
obliterated.
Identify the suprasellar and quadrigeminal cisterns in
the following examples.
View moderately increased ICP.
 The suprasellar cistern is slightly smaller than its
normal size (the right uncus is pushing into the
suprasellar cistern) and the quadrigeminal cistern is
compressed. An epidural hematoma is noted.
View severe ICP increase.
The suprasellar cistern is slightly smaller than its
normal size (the right uncus is pushing into the
suprasellar cistern) and the quadrigeminal cistern is
compressed. An epidural hematoma is noted.
View severe ICP increase.
 The suprasellar cistern (left image) is tissue-filled,
indicating the presence of brain tissue herniating into
this space. The quadrigeminal cistern is very
compressed and pushed posteriorly (center image).
The suprasellar cistern is located just above the base of
the skull (above the sella). It should be visible in the
cuts near the base of the brain. If it is not visible, it
suggests that the suprasellar cistern is obliterated.
Similarly, the quadrigeminal cistern should be located in
the cut above the suprasellar cistern. A subdural
hematoma is noted with a midline shift.
Brain Herniation Syndromes:
1. Uncal herniation:
When mass effects within or adjacent to the
temporal lobe occur, the medial portion of the temporal
lobe (uncus) is forced medially and downward over the
tentorium. There is ipsilateral pupillary dilation. The
uncus is pushed medially into the suprasellar cistern.
View uncal herniation.
The suprasellar cistern (left image) is tissue-filled,
indicating the presence of brain tissue herniating into
this space. The quadrigeminal cistern is very
compressed and pushed posteriorly (center image).
The suprasellar cistern is located just above the base of
the skull (above the sella). It should be visible in the
cuts near the base of the brain. If it is not visible, it
suggests that the suprasellar cistern is obliterated.
Similarly, the quadrigeminal cistern should be located in
the cut above the suprasellar cistern. A subdural
hematoma is noted with a midline shift.
Brain Herniation Syndromes:
1. Uncal herniation:
When mass effects within or adjacent to the
temporal lobe occur, the medial portion of the temporal
lobe (uncus) is forced medially and downward over the
tentorium. There is ipsilateral pupillary dilation. The
uncus is pushed medially into the suprasellar cistern.
View uncal herniation.
 There is bilateral uncal herniation. The suprasellar
cistern is obliterated.
View early uncal herniation.
There is bilateral uncal herniation. The suprasellar
cistern is obliterated.
View early uncal herniation.
 The right uncus is pushing into the suprasellar
cistern; early right uncal herniation.
2. Transtentorial herniation:
It should be noted that this term is somewhat vague.
It is used rather loosely and it may sometimes be used
similarly to the terms temporal lobe herniation and uncal
herniation. The uncus may herniate over the tentorium
as described above. Supratentorial lesions on one side
may initially result in uncal herniation. As ICP increases
further, bilateral temporal lobe herniation occurs
transtentorially. Early unilateral uncal herniation is
more accurately called uncal herniation. The terms
cranial-caudal transtentorial herniation, rostro-caudal
transtentorial herniation, or central transtentorial
herniation more accurately describe what is generally
meant by "transtentorial herniation". Thus, uncal
herniation is described separately above.
In transtentorial herniation the medial portions of the
temporal lobes (uncus) and the brainstem herniate
downward from supratentorial to the infratentorial
compartment. The clinical signs include headache,
decreasing level of consciousness and ipsilateral fixed
dilated pupil (from compression of the third cranial
nerve on the ipsilateral side). As herniation worsens,
decerebrate (extensor) posturing, contralateral (ie.,
bilateral) pupillary dilation and Cushing's triad occur.
Cushing's triad includes alteration in respiration,
bradycardia, and systemic hypertension. It is rare to
have all three present in children. Often there is just
bradycardia alone. Children tolerate brainstem
compression produced by herniation better than adults.
Immediate early intervention can result in recovery.
Intervention at the stage of unilateral pupillary
dysfunction is likely to have a better prognosis
than intervention at the stage of bilateral pupillary
dysfunction, decerebrate posturing and bradycardia.
CT scan shows obliteration of the suprasellar and
quadrigeminal cisterns. Later findings include infarcts
and brainstem hemorrhage.
View transtentorial herniation.
The right uncus is pushing into the suprasellar
cistern; early right uncal herniation.
2. Transtentorial herniation:
It should be noted that this term is somewhat vague.
It is used rather loosely and it may sometimes be used
similarly to the terms temporal lobe herniation and uncal
herniation. The uncus may herniate over the tentorium
as described above. Supratentorial lesions on one side
may initially result in uncal herniation. As ICP increases
further, bilateral temporal lobe herniation occurs
transtentorially. Early unilateral uncal herniation is
more accurately called uncal herniation. The terms
cranial-caudal transtentorial herniation, rostro-caudal
transtentorial herniation, or central transtentorial
herniation more accurately describe what is generally
meant by "transtentorial herniation". Thus, uncal
herniation is described separately above.
In transtentorial herniation the medial portions of the
temporal lobes (uncus) and the brainstem herniate
downward from supratentorial to the infratentorial
compartment. The clinical signs include headache,
decreasing level of consciousness and ipsilateral fixed
dilated pupil (from compression of the third cranial
nerve on the ipsilateral side). As herniation worsens,
decerebrate (extensor) posturing, contralateral (ie.,
bilateral) pupillary dilation and Cushing's triad occur.
Cushing's triad includes alteration in respiration,
bradycardia, and systemic hypertension. It is rare to
have all three present in children. Often there is just
bradycardia alone. Children tolerate brainstem
compression produced by herniation better than adults.
Immediate early intervention can result in recovery.
Intervention at the stage of unilateral pupillary
dysfunction is likely to have a better prognosis
than intervention at the stage of bilateral pupillary
dysfunction, decerebrate posturing and bradycardia.
CT scan shows obliteration of the suprasellar and
quadrigeminal cisterns. Later findings include infarcts
and brainstem hemorrhage.
View transtentorial herniation.
 The suprasellar cistern (left image) is obliterated.
The quadrigeminal cistern is very compressed and
pushed posteriorly (center image). A subdural
hematoma with a midline shift is noted. There is central
transtentorial and subfalcine herniation.
3. Tonsillar herniation:
In tonsillar herniation (rare), a mass effect in the
posterior fossa causes the cerebellar tonsils to
herniate inferiorly through the foramen magnum
compressing the medulla and upper cervical spinal
cord. Conscious patients complain of neck pain and
vomiting. They may have nystagmus, pupillary
dilatation, bradycardia, hypertension and respiratory
depression. Early tonsillar herniation is difficult to
recognize in an unconscious patient. It may not be
evident on CT scan since axial views cannot see the
pathology well. It is best seen on sagittal MRI.
Clinically changes in vital signs may be the only clinical
clue in an unconscious patient.
4. Subfalcine herniation (cingulate herniation):
A unilateral supratentorial mass or hemorrhage
results in a midline shift. If the pressure pushing the
brain to one side is great enough, one of the
hemispheres is pushed under the falx (subfalcine). This
may compress the anterior cerebral artery. There is
ipsilateral lateral ventricle compression and
contralateral lateral ventricle dilation (due to obstruction
of the foramen of Monroe).
View subfalcine herniation.
The suprasellar cistern (left image) is obliterated.
The quadrigeminal cistern is very compressed and
pushed posteriorly (center image). A subdural
hematoma with a midline shift is noted. There is central
transtentorial and subfalcine herniation.
3. Tonsillar herniation:
In tonsillar herniation (rare), a mass effect in the
posterior fossa causes the cerebellar tonsils to
herniate inferiorly through the foramen magnum
compressing the medulla and upper cervical spinal
cord. Conscious patients complain of neck pain and
vomiting. They may have nystagmus, pupillary
dilatation, bradycardia, hypertension and respiratory
depression. Early tonsillar herniation is difficult to
recognize in an unconscious patient. It may not be
evident on CT scan since axial views cannot see the
pathology well. It is best seen on sagittal MRI.
Clinically changes in vital signs may be the only clinical
clue in an unconscious patient.
4. Subfalcine herniation (cingulate herniation):
A unilateral supratentorial mass or hemorrhage
results in a midline shift. If the pressure pushing the
brain to one side is great enough, one of the
hemispheres is pushed under the falx (subfalcine). This
may compress the anterior cerebral artery. There is
ipsilateral lateral ventricle compression and
contralateral lateral ventricle dilation (due to obstruction
of the foramen of Monroe).
View subfalcine herniation.
 The suprasellar cistern (left image) is obliterated.
The quadrigeminal cistern is very compressed and
pushed posteriorly (center image). A subdural
hematoma with a midline shift is noted. There is central
transtentorial and subfalcine herniation.
5. Superior vermian herniation:
Also called ascending transtentorial herniation, this
involves upward herniation of the vermis and cerebellar
hemispheres through the tentorial incisura due to a
mass effect in the posterior fossa. There is effacement
of the quadrigeminal cistern. There is hydrocephalus
due to compression of the aqueduct of Sylvius.
References
Grossman RI, Yousem DM. Head Trauma. In:
Grossman RI, Yousem DM. Neuroradiology - The
Requisites. Mosby, St. Louis, 1994, pp. 149-169.
Bruce DA. Head Trauma. In: Fleisher GR, Ludwig
S (eds). Textbook of Pediatric Emergency Medicine,
3rd ed. Williams & Wilkins, Philadelphia, 1993. pp.
1102-1119.
Kirkwood RJ. Head Trauma. In: Kirkwood JR.
Essentials of Neuroimaging, second edition. Churchill
Livingstone, New York, 1995, pp. 339-359.
Truwit CL, Lempert TE. High Resolution Atlas of
Cranial Neuroanatomy. Williams & Wilkins, Baltimore,
1994.
Willing SJ. General Manifestations of Intracranial
Diseases. In: Willing SJ. Atlas of Neuroradiology.
W.B Saunders, Philadelphia, 1995, pp. 1-40.
Castillo M, Harris JH. Skull and Brain. In: Harris
JH, Harris WH, Novelline RA (eds). The Radiology of
Emergency Medicine. Williams & Wilkins, Baltimore,
1993, pp. 1-35.
The suprasellar cistern (left image) is obliterated.
The quadrigeminal cistern is very compressed and
pushed posteriorly (center image). A subdural
hematoma with a midline shift is noted. There is central
transtentorial and subfalcine herniation.
5. Superior vermian herniation:
Also called ascending transtentorial herniation, this
involves upward herniation of the vermis and cerebellar
hemispheres through the tentorial incisura due to a
mass effect in the posterior fossa. There is effacement
of the quadrigeminal cistern. There is hydrocephalus
due to compression of the aqueduct of Sylvius.
References
Grossman RI, Yousem DM. Head Trauma. In:
Grossman RI, Yousem DM. Neuroradiology - The
Requisites. Mosby, St. Louis, 1994, pp. 149-169.
Bruce DA. Head Trauma. In: Fleisher GR, Ludwig
S (eds). Textbook of Pediatric Emergency Medicine,
3rd ed. Williams & Wilkins, Philadelphia, 1993. pp.
1102-1119.
Kirkwood RJ. Head Trauma. In: Kirkwood JR.
Essentials of Neuroimaging, second edition. Churchill
Livingstone, New York, 1995, pp. 339-359.
Truwit CL, Lempert TE. High Resolution Atlas of
Cranial Neuroanatomy. Williams & Wilkins, Baltimore,
1994.
Willing SJ. General Manifestations of Intracranial
Diseases. In: Willing SJ. Atlas of Neuroradiology.
W.B Saunders, Philadelphia, 1995, pp. 1-40.
Castillo M, Harris JH. Skull and Brain. In: Harris
JH, Harris WH, Novelline RA (eds). The Radiology of
Emergency Medicine. Williams & Wilkins, Baltimore,
1993, pp. 1-35.