Shoulder Pain After Throwing a Football
Radiology Cases in Pediatric Emergency Medicine
Volume 6, Case 1
Loren G. Yamamoto, MD, MPH
Kapiolani Medical Center For Women And Children
University of Hawaii John A. Burns School of Medicine
This is a 10-year old male who was throwing a
football with his friends in the morning while at a youth
camp. He noted some shoulder pain following this
which worsened through the afternoon. The pain was
not of sudden onset and it did not feel like his shoulder
popped out. He did not fall onto his shoulder and he
was not struck in the shoulder by anyone. He was
brought to the emergency department because of
persistent pain and limited movement of his shoulder.
He denied any numbness or tingling.
His past history is unremarkable. Specifically, it is
negative for any fractures.
Exam: VS T37.3, P80, R18, BP 120/70. He is alert
and comfortable in no distress. His anterior left
shoulder is swollen. The head of the humerus is
prominent anteriorly. There is severe tenderness in this
region. There is tenderness along the entire humerus.
His clavicle is non-tender. He is not tender over the
elbow. Supination and pronation are intact. There is
no visible deformity other than the shoulder. Pulses,
perfusion, sensation and finger movement are all intact
distally. The remainder of his physical exam is
unremarkable.
What is his diagnosis clinically? Should we attempt
to reduce a possible shoulder dislocation without
obtaining radiographs? This does not appear to be a
shoulder dislocation since there is no sudden event
causing the dislocation. While throwing can cause a
dislocation, his history is not consistent with this.
Additionally, shoulder dislocations in young children are
not very common, while fractures are fairly common. It
would be best to obtain radiographs first.
What would radiographs reveal in such a patient? Is
a fracture possible? According to his history, his
shoulder does not appear to have sustained enough
trauma to cause a fracture and the gradual onset and
progression of his pain does not appear to be
consistent with a fracture. We often make such
assumptions, but we are often assuming that every
patient has normal bones. Patients occasionally have
bone abnormalities such as metastatic tumor, bone
cysts or occult primary bone diseases which make the
patient's bone highly fracture prone. Without
radiographs, we would not be able to tell if there is an
abnormality of the bone. In addition to this uncertainty,
the history given to us may be incorrect. Histories are
frequently fabricated as a cover-up for child abuse.
Radiographs of his shoulder are obtained.
View shoulder radiographs.
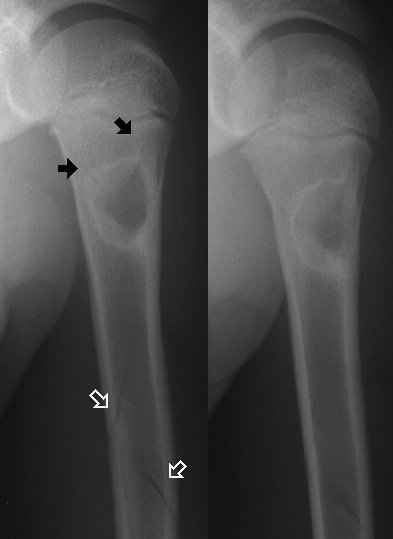
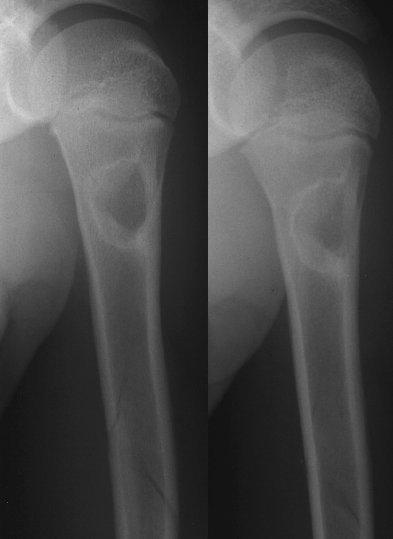 These radiographs demonstrate a pathologic
fracture through a bone cyst of the proximal humerus.
The fracture extends distally through the humerus. The
bone cyst's margins are well defined and slightly
sclerotic.
View pointers.
These radiographs demonstrate a pathologic
fracture through a bone cyst of the proximal humerus.
The fracture extends distally through the humerus. The
bone cyst's margins are well defined and slightly
sclerotic.
View pointers.
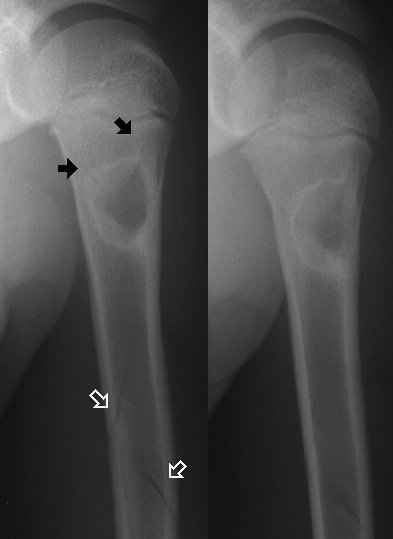 The black arrows point out the fractures around the
cyst. The white outline arrows point out the fractures in
the mid humerus.
If the clinician assumes that a fracture is not
possible and attempts to reduce a dislocated shoulder,
this would worsen a fracture injury and cause
unnecessary pain. You may decide to assume that
your patient has normal bones, but this is not always
true.
In another case, a 9 year old boy presents with
severe shoulder pain after bumping his shoulder
against a door as the door was closing. Radiographs
are obtained.
View shoulder radiographs.
The black arrows point out the fractures around the
cyst. The white outline arrows point out the fractures in
the mid humerus.
If the clinician assumes that a fracture is not
possible and attempts to reduce a dislocated shoulder,
this would worsen a fracture injury and cause
unnecessary pain. You may decide to assume that
your patient has normal bones, but this is not always
true.
In another case, a 9 year old boy presents with
severe shoulder pain after bumping his shoulder
against a door as the door was closing. Radiographs
are obtained.
View shoulder radiographs.

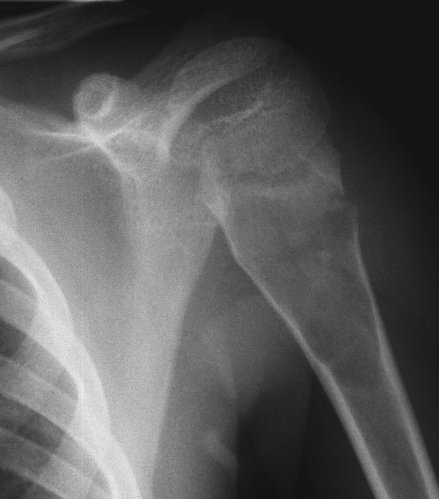
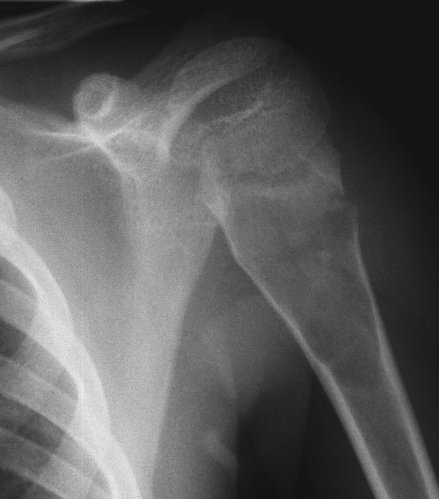 These radiographs show a large bone cyst in the
proximal humerus with a pathologic fracture involving
the cyst. This is another case where the history of the
trauma is minor, but a fracture is present because of
abnormal bone. We cannot always assume that our
patients have normal bones.
Pathologic fractures occur with minimal trauma that
would not ordinarily be expected to cause a fracture.
Basically, these are fractures through weak bones.
Conditions causing weak bones can be divided into two
types: 1) conditions which cause focal weakness and
2) generalized conditions causing all the bones to be
weak.
Focal conditions include benign tumors or tumor-like
conditions, malignant bone tumors, metastatic lesions,
infectious or inflammatory conditions (osteomyelitis,
eosinophillic granuloma) and iatrogenically weakened
areas of bone (screw holes, bone graft harvest sites,
etc.). While an incompletely healed fracture may be
weaker than normal bone, a new fracture through a
healing fracture is generally not considered to be a
pathologic fracture.
Generalized conditions resulting in weak bones
include osteogenesis imperfecta, osteopetrosis,
neurofibromatosis, fibrous dysplasia, rickets, renal
osteodystrophy, scurvy, hyperparathyroidism, Cushing's
syndrome, cytotoxic drugs and disuse atrophy due to
neurological or other disabling conditions resulting in
generalized demineralization.
Unicameral bone cysts are one of the most common
types of benign bone cysts. These cysts contain
serous fluid and are lined by a thin connective tissue
membrane. Most of these are located in the
metaphysis of the proximal humerus or femur. These
usually heal spontaneously during the teen years unless
a pathologic fracture occurs. Large cysts at risk for
recurrent pathologic fracture require treatment, while
smaller lesions generally regress on their own.
Aneurysmal bone cysts are also benign bone cysts,
but are not as common as unicameral bone cysts.
Common locations include the spine and the same
areas as unicameral bone cysts. These are
eccentrically placed within the metaphysis. The lesion
resorbs cortex and elevates the periosteum resulting in
an aneurysm-like appearance. These are more difficult
to distinguish from malignant tumors and CT may be
helpful in determining this.
Non-ossifying fibromas, non-osteogenic fibromas
and fibrous cortical defects are different terms for the
same histologic process (synonyms). The names differ
because of the different radiographic appearances.
Small lesions are called fibrous cortical defects. Larger
lesions, referred to as non-ossifying fibromas, cause
bulging of the bone and bony reaction over the lesion.
Fibrous dysplasia is a developmental anomaly of
the bone that results in focal lesions of the bone where
fibrous tissue replaces the medullary canal. The
majority of patients have a single focal lesion and a few
patients have multiple lesions.
References:
Poitras B, Rivard CH. Pathologic Fractures
(Chapter 56). In: Letts RM (ed). Management of
Pediatric Fractures, New York, New York, Churchill
Livingstone, 1994, pp. 1027-1048.
These radiographs show a large bone cyst in the
proximal humerus with a pathologic fracture involving
the cyst. This is another case where the history of the
trauma is minor, but a fracture is present because of
abnormal bone. We cannot always assume that our
patients have normal bones.
Pathologic fractures occur with minimal trauma that
would not ordinarily be expected to cause a fracture.
Basically, these are fractures through weak bones.
Conditions causing weak bones can be divided into two
types: 1) conditions which cause focal weakness and
2) generalized conditions causing all the bones to be
weak.
Focal conditions include benign tumors or tumor-like
conditions, malignant bone tumors, metastatic lesions,
infectious or inflammatory conditions (osteomyelitis,
eosinophillic granuloma) and iatrogenically weakened
areas of bone (screw holes, bone graft harvest sites,
etc.). While an incompletely healed fracture may be
weaker than normal bone, a new fracture through a
healing fracture is generally not considered to be a
pathologic fracture.
Generalized conditions resulting in weak bones
include osteogenesis imperfecta, osteopetrosis,
neurofibromatosis, fibrous dysplasia, rickets, renal
osteodystrophy, scurvy, hyperparathyroidism, Cushing's
syndrome, cytotoxic drugs and disuse atrophy due to
neurological or other disabling conditions resulting in
generalized demineralization.
Unicameral bone cysts are one of the most common
types of benign bone cysts. These cysts contain
serous fluid and are lined by a thin connective tissue
membrane. Most of these are located in the
metaphysis of the proximal humerus or femur. These
usually heal spontaneously during the teen years unless
a pathologic fracture occurs. Large cysts at risk for
recurrent pathologic fracture require treatment, while
smaller lesions generally regress on their own.
Aneurysmal bone cysts are also benign bone cysts,
but are not as common as unicameral bone cysts.
Common locations include the spine and the same
areas as unicameral bone cysts. These are
eccentrically placed within the metaphysis. The lesion
resorbs cortex and elevates the periosteum resulting in
an aneurysm-like appearance. These are more difficult
to distinguish from malignant tumors and CT may be
helpful in determining this.
Non-ossifying fibromas, non-osteogenic fibromas
and fibrous cortical defects are different terms for the
same histologic process (synonyms). The names differ
because of the different radiographic appearances.
Small lesions are called fibrous cortical defects. Larger
lesions, referred to as non-ossifying fibromas, cause
bulging of the bone and bony reaction over the lesion.
Fibrous dysplasia is a developmental anomaly of
the bone that results in focal lesions of the bone where
fibrous tissue replaces the medullary canal. The
majority of patients have a single focal lesion and a few
patients have multiple lesions.
References:
Poitras B, Rivard CH. Pathologic Fractures
(Chapter 56). In: Letts RM (ed). Management of
Pediatric Fractures, New York, New York, Churchill
Livingstone, 1994, pp. 1027-1048.
Return to Radiology Cases In Ped Emerg Med Case Selection Page
Return to Univ. Hawaii Dept. Pediatrics Home Page
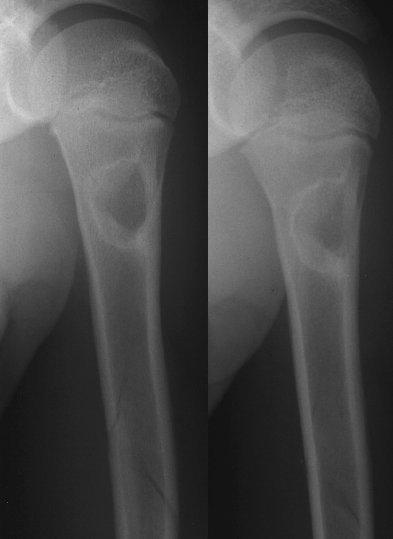 These radiographs demonstrate a pathologic
fracture through a bone cyst of the proximal humerus.
The fracture extends distally through the humerus. The
bone cyst's margins are well defined and slightly
sclerotic.
View pointers.
These radiographs demonstrate a pathologic
fracture through a bone cyst of the proximal humerus.
The fracture extends distally through the humerus. The
bone cyst's margins are well defined and slightly
sclerotic.
View pointers.
 The black arrows point out the fractures around the
cyst. The white outline arrows point out the fractures in
the mid humerus.
If the clinician assumes that a fracture is not
possible and attempts to reduce a dislocated shoulder,
this would worsen a fracture injury and cause
unnecessary pain. You may decide to assume that
your patient has normal bones, but this is not always
true.
In another case, a 9 year old boy presents with
severe shoulder pain after bumping his shoulder
against a door as the door was closing. Radiographs
are obtained.
View shoulder radiographs.
The black arrows point out the fractures around the
cyst. The white outline arrows point out the fractures in
the mid humerus.
If the clinician assumes that a fracture is not
possible and attempts to reduce a dislocated shoulder,
this would worsen a fracture injury and cause
unnecessary pain. You may decide to assume that
your patient has normal bones, but this is not always
true.
In another case, a 9 year old boy presents with
severe shoulder pain after bumping his shoulder
against a door as the door was closing. Radiographs
are obtained.
View shoulder radiographs.

 These radiographs show a large bone cyst in the
proximal humerus with a pathologic fracture involving
the cyst. This is another case where the history of the
trauma is minor, but a fracture is present because of
abnormal bone. We cannot always assume that our
patients have normal bones.
Pathologic fractures occur with minimal trauma that
would not ordinarily be expected to cause a fracture.
Basically, these are fractures through weak bones.
Conditions causing weak bones can be divided into two
types: 1) conditions which cause focal weakness and
2) generalized conditions causing all the bones to be
weak.
Focal conditions include benign tumors or tumor-like
conditions, malignant bone tumors, metastatic lesions,
infectious or inflammatory conditions (osteomyelitis,
eosinophillic granuloma) and iatrogenically weakened
areas of bone (screw holes, bone graft harvest sites,
etc.). While an incompletely healed fracture may be
weaker than normal bone, a new fracture through a
healing fracture is generally not considered to be a
pathologic fracture.
Generalized conditions resulting in weak bones
include osteogenesis imperfecta, osteopetrosis,
neurofibromatosis, fibrous dysplasia, rickets, renal
osteodystrophy, scurvy, hyperparathyroidism, Cushing's
syndrome, cytotoxic drugs and disuse atrophy due to
neurological or other disabling conditions resulting in
generalized demineralization.
Unicameral bone cysts are one of the most common
types of benign bone cysts. These cysts contain
serous fluid and are lined by a thin connective tissue
membrane. Most of these are located in the
metaphysis of the proximal humerus or femur. These
usually heal spontaneously during the teen years unless
a pathologic fracture occurs. Large cysts at risk for
recurrent pathologic fracture require treatment, while
smaller lesions generally regress on their own.
Aneurysmal bone cysts are also benign bone cysts,
but are not as common as unicameral bone cysts.
Common locations include the spine and the same
areas as unicameral bone cysts. These are
eccentrically placed within the metaphysis. The lesion
resorbs cortex and elevates the periosteum resulting in
an aneurysm-like appearance. These are more difficult
to distinguish from malignant tumors and CT may be
helpful in determining this.
Non-ossifying fibromas, non-osteogenic fibromas
and fibrous cortical defects are different terms for the
same histologic process (synonyms). The names differ
because of the different radiographic appearances.
Small lesions are called fibrous cortical defects. Larger
lesions, referred to as non-ossifying fibromas, cause
bulging of the bone and bony reaction over the lesion.
Fibrous dysplasia is a developmental anomaly of
the bone that results in focal lesions of the bone where
fibrous tissue replaces the medullary canal. The
majority of patients have a single focal lesion and a few
patients have multiple lesions.
References:
Poitras B, Rivard CH. Pathologic Fractures
(Chapter 56). In: Letts RM (ed). Management of
Pediatric Fractures, New York, New York, Churchill
Livingstone, 1994, pp. 1027-1048.
These radiographs show a large bone cyst in the
proximal humerus with a pathologic fracture involving
the cyst. This is another case where the history of the
trauma is minor, but a fracture is present because of
abnormal bone. We cannot always assume that our
patients have normal bones.
Pathologic fractures occur with minimal trauma that
would not ordinarily be expected to cause a fracture.
Basically, these are fractures through weak bones.
Conditions causing weak bones can be divided into two
types: 1) conditions which cause focal weakness and
2) generalized conditions causing all the bones to be
weak.
Focal conditions include benign tumors or tumor-like
conditions, malignant bone tumors, metastatic lesions,
infectious or inflammatory conditions (osteomyelitis,
eosinophillic granuloma) and iatrogenically weakened
areas of bone (screw holes, bone graft harvest sites,
etc.). While an incompletely healed fracture may be
weaker than normal bone, a new fracture through a
healing fracture is generally not considered to be a
pathologic fracture.
Generalized conditions resulting in weak bones
include osteogenesis imperfecta, osteopetrosis,
neurofibromatosis, fibrous dysplasia, rickets, renal
osteodystrophy, scurvy, hyperparathyroidism, Cushing's
syndrome, cytotoxic drugs and disuse atrophy due to
neurological or other disabling conditions resulting in
generalized demineralization.
Unicameral bone cysts are one of the most common
types of benign bone cysts. These cysts contain
serous fluid and are lined by a thin connective tissue
membrane. Most of these are located in the
metaphysis of the proximal humerus or femur. These
usually heal spontaneously during the teen years unless
a pathologic fracture occurs. Large cysts at risk for
recurrent pathologic fracture require treatment, while
smaller lesions generally regress on their own.
Aneurysmal bone cysts are also benign bone cysts,
but are not as common as unicameral bone cysts.
Common locations include the spine and the same
areas as unicameral bone cysts. These are
eccentrically placed within the metaphysis. The lesion
resorbs cortex and elevates the periosteum resulting in
an aneurysm-like appearance. These are more difficult
to distinguish from malignant tumors and CT may be
helpful in determining this.
Non-ossifying fibromas, non-osteogenic fibromas
and fibrous cortical defects are different terms for the
same histologic process (synonyms). The names differ
because of the different radiographic appearances.
Small lesions are called fibrous cortical defects. Larger
lesions, referred to as non-ossifying fibromas, cause
bulging of the bone and bony reaction over the lesion.
Fibrous dysplasia is a developmental anomaly of
the bone that results in focal lesions of the bone where
fibrous tissue replaces the medullary canal. The
majority of patients have a single focal lesion and a few
patients have multiple lesions.
References:
Poitras B, Rivard CH. Pathologic Fractures
(Chapter 56). In: Letts RM (ed). Management of
Pediatric Fractures, New York, New York, Churchill
Livingstone, 1994, pp. 1027-1048.