Orbital Injury
Radiology Cases in Pediatric Emergency Medicine
Volume 6, Case 9
Brunhild Halm, MD, PhD
Kapiolani Medical Center For Women And Children
University of Hawaii John A. Burns School of Medicine
This is an 8 year old boy who was playing with his
brother who accidentally kicked him in the left side of
the face with his knee. The boy developed epistaxis
immediately after the injury and he complained of
intermittent double vision in his left eye. He did not
loose consciousness, but his parents noted increased
somnolence and 3 episodes of emesis.
Past medical history is negative.
Exam: VS T36.6, HR 90, RR 16, BP 137/83,
oxygen saturation 100% in room air. He is somnolent,
but easily arousable. Eyes: Visual acuity 20/25 OU.
There is no proptosis. There is ecchymosis and
swelling of his left lower eyelid. There is mild left
periorbital swelling but no obvious tenderness or step
off deformity on palpation. The cornea, lens and
anterior chamber are clear. There is no hyphema.
Pupils are equal and reactive. There is restricted
upward and downward gaze in his left eye, but normal
ab/adduction. EOM's are normal in the right eye.
Sensation in the distribution of the infraorbital nerve is
intact.
TM's clear, no blood. There is blood in his nares.
No septal swelling is noted. His pharynx is clear. His
neck is nontender with full range of motion. His chest
is clear to auscultation. Heart regular without murmurs.
Abdomen nontender with active bowel sounds. His
speech is normal. Deep tendon reflexes are normal.
His strength is normal.
A CT scan of the brain and orbits is obtained.
View CT scan.
 The brain is normal. The CT cut shown is taken in
the axial projection (i.e., the long axis of his body is
perpendicular to the plane of the CT scanner) through
the orbits using a "bone window" contrast setting. The
black arrow points to the medial wall of the left orbit
which is fractured and pushed medially.
Additional coronal CT views are taken of the orbits
by hyperextending his neck so that the long axis of his
head is closer to being parallel with the plane of the CT
scanner. Since axial cuts are parallel with the floor of
the orbit, some fractures of the orbital floor are not well
visualized. By repositioning the patient so that the CT
cuts are perpendicular to the orbital floor, a fracture of
the orbital floor can be more accurately visualized.
View coronal CT cut.
The brain is normal. The CT cut shown is taken in
the axial projection (i.e., the long axis of his body is
perpendicular to the plane of the CT scanner) through
the orbits using a "bone window" contrast setting. The
black arrow points to the medial wall of the left orbit
which is fractured and pushed medially.
Additional coronal CT views are taken of the orbits
by hyperextending his neck so that the long axis of his
head is closer to being parallel with the plane of the CT
scanner. Since axial cuts are parallel with the floor of
the orbit, some fractures of the orbital floor are not well
visualized. By repositioning the patient so that the CT
cuts are perpendicular to the orbital floor, a fracture of
the orbital floor can be more accurately visualized.
View coronal CT cut.
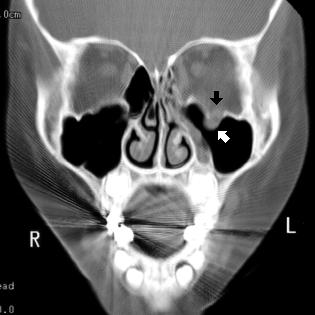 These coronal views reveal a fracture of the left
orbital floor (black arrow). The white arrow points to the
inferior rectus muscle protruding into the maxillary
sinus through the orbital floor fracture site. The clinical
findings suggest that there may be entrapment of the
left inferior rectus muscle, leading to restriction in
upward and downward gaze and diplopia when trying to
look in these directions. The small depressed fracture
of the medial wall of the left orbit with opacification of
the left ethmoid air cells is again visible.
Fractures of the orbital floor may be difficult to
visualize on an axial CT scan through the orbits since
the orbital floor is parallel to the plane of the scan.
Fractures are best seen when the fracture is
perpendicular or oblique to the plane of the scan.
Thus, when an orbital floor fracture is suspected, as in
trauma to the orbit, coronal scans of the orbit should be
obtained, provided that the patient can be positioned
properly.
Orbital wall fractures:
The orbital bones are very delicate and their
thickness is similar to that of an eggshell. Orbital wall
fractures most often occur in the orbital floor and
sometimes in the medial wall, because these are the
weakest regions of the bony orbit. The proximity of the
paranasal sinuses, nerves, vessels, extraocular
muscles, globe and other orbital structures predispose
them to a wide variety of possible damage from injury
producing orbital fractures.
An orbital blow out fracture refers to a fracture of the
orbital floor, usually without involvement of the orbital
rim. The impacting object typically has a diameter that
is larger than that of the orbital opening. Examples
include a fist, tennis ball, baseball, snowball or door
knob. The mechanism of a blow out fracture is
controversial. There are two main theories that are
likely: 1) The fracture results from a sudden increase in
intraorbital pressure when the globe is being pushed
posteriorly. 2) The fracture is the result of "buckling"
forces which are transmitted to the orbital bones by
transient deformity of the orbital rim.
An aide to the evaluation of children with orbital
fractures is the mnemonic HEADER:
Hyphema: Evaluate the child for bleeding in the
anterior chamber and for other intraocular injuries.
Emphysema: Orbital emphysema is due to a
fracture of the medial wall and/or inferior wall which
permits communication between the ethmoid sinus
and/or the maxillary sinus with the orbital contents. In
order to make the diagnosis of orbital emphysema
clinically, the orbit should be palpated for crepitus.
Subcutaneous air can be dramatic when the patient
blows his/her nose. Patients may notice eye swelling
when blowing their nose. Orbital emphysema may be
visible on a plain radiograph of the orbit. It is also
visible on CT scans.
Epistaxis: A fracture of the medial orbital wall can
result in a significant nose bleed.
Anesthesia or hypoaesthesia in the distribution of
the second branch of the trigeminal nerve must be
suspected in any fracture involving the infraorbital
canal. The distribution involves the lower eyelid and
the cheek down to the upper lip on the side of the
injury.
Diplopia: Double vision has essentially two primary
mechanisms: 1) A mechanical entrapment of an eye
muscle, most commonly, the inferior rectus muscle, or
the inferior oblique muscle. 2) A paralytic component
where injury to the third cranial nerve has occurred.
The third cranial nerve innervates both the inferior
rectus and the inferior oblique muscle. Hemorrhage
and edema within the extraocular muscles may also
cause transient paresis.
Exophthalmos is secondary to intraorbital
hemorrhage and edema which pushes the globe
anteriorly. However, a large fracture of the medial
wall or orbital floor may result in enophthalmos.
Restriction: Entrapment of extraocular muscles and
orbital tissue in the fracture site leads to decreased
ocular motility. With orbital floor fractures, the inferior
rectus muscle most commonly is entrapped leading to
limitation in upward gaze. With medial wall fractures,
limited abduction due to medial rectus incarceration
may result.
Diagnosis:
CT scanning is highly useful in the assessment of
orbital trauma and associated injures to the brain and
sinuses. Coronal views (direct or reconstructed) should
be requested when orbital trauma is present.
Plain radiographs are not sufficient. They may be
helpful in confirming fractures and in the delineation of
air-fluid levels in the paranasal sinuses, but they may
fail to show the existence and extent of orbital
fractures.
Surgical repair of a fractured orbital wall would be
indicated in the following instances: 1) Significant
enophthalmos. 2) Diplopia in primary gaze or in a
functional gaze. 3) Significant limitation of extraocular
movements.
References:
1. Levin AV. Eye trauma. In: Fleisher GR, Ludwig
S (eds). Textbook of Pediatric Emergency Medicine,
3rd edition. 1993, Baltimore, MD, Williams and
Wilkins, pp. 1200-1209.
2. Mead MD. Evaluation and Initial Management of
Patients with Ocular and Adnexal Trauma. In: Albert
DM, Jakobiec FA (eds). Principles and Practice of
Ophthalmology. 1994, Philadelphia, Saunders, Volume
5, pp. 3362-3375.
3. Friendly DS, Jaafar MS. Ocular Trauma. In:
Eichelberger MR. Pediatric Trauma. 1993, St. Louis,
pp. 401-410.
These coronal views reveal a fracture of the left
orbital floor (black arrow). The white arrow points to the
inferior rectus muscle protruding into the maxillary
sinus through the orbital floor fracture site. The clinical
findings suggest that there may be entrapment of the
left inferior rectus muscle, leading to restriction in
upward and downward gaze and diplopia when trying to
look in these directions. The small depressed fracture
of the medial wall of the left orbit with opacification of
the left ethmoid air cells is again visible.
Fractures of the orbital floor may be difficult to
visualize on an axial CT scan through the orbits since
the orbital floor is parallel to the plane of the scan.
Fractures are best seen when the fracture is
perpendicular or oblique to the plane of the scan.
Thus, when an orbital floor fracture is suspected, as in
trauma to the orbit, coronal scans of the orbit should be
obtained, provided that the patient can be positioned
properly.
Orbital wall fractures:
The orbital bones are very delicate and their
thickness is similar to that of an eggshell. Orbital wall
fractures most often occur in the orbital floor and
sometimes in the medial wall, because these are the
weakest regions of the bony orbit. The proximity of the
paranasal sinuses, nerves, vessels, extraocular
muscles, globe and other orbital structures predispose
them to a wide variety of possible damage from injury
producing orbital fractures.
An orbital blow out fracture refers to a fracture of the
orbital floor, usually without involvement of the orbital
rim. The impacting object typically has a diameter that
is larger than that of the orbital opening. Examples
include a fist, tennis ball, baseball, snowball or door
knob. The mechanism of a blow out fracture is
controversial. There are two main theories that are
likely: 1) The fracture results from a sudden increase in
intraorbital pressure when the globe is being pushed
posteriorly. 2) The fracture is the result of "buckling"
forces which are transmitted to the orbital bones by
transient deformity of the orbital rim.
An aide to the evaluation of children with orbital
fractures is the mnemonic HEADER:
Hyphema: Evaluate the child for bleeding in the
anterior chamber and for other intraocular injuries.
Emphysema: Orbital emphysema is due to a
fracture of the medial wall and/or inferior wall which
permits communication between the ethmoid sinus
and/or the maxillary sinus with the orbital contents. In
order to make the diagnosis of orbital emphysema
clinically, the orbit should be palpated for crepitus.
Subcutaneous air can be dramatic when the patient
blows his/her nose. Patients may notice eye swelling
when blowing their nose. Orbital emphysema may be
visible on a plain radiograph of the orbit. It is also
visible on CT scans.
Epistaxis: A fracture of the medial orbital wall can
result in a significant nose bleed.
Anesthesia or hypoaesthesia in the distribution of
the second branch of the trigeminal nerve must be
suspected in any fracture involving the infraorbital
canal. The distribution involves the lower eyelid and
the cheek down to the upper lip on the side of the
injury.
Diplopia: Double vision has essentially two primary
mechanisms: 1) A mechanical entrapment of an eye
muscle, most commonly, the inferior rectus muscle, or
the inferior oblique muscle. 2) A paralytic component
where injury to the third cranial nerve has occurred.
The third cranial nerve innervates both the inferior
rectus and the inferior oblique muscle. Hemorrhage
and edema within the extraocular muscles may also
cause transient paresis.
Exophthalmos is secondary to intraorbital
hemorrhage and edema which pushes the globe
anteriorly. However, a large fracture of the medial
wall or orbital floor may result in enophthalmos.
Restriction: Entrapment of extraocular muscles and
orbital tissue in the fracture site leads to decreased
ocular motility. With orbital floor fractures, the inferior
rectus muscle most commonly is entrapped leading to
limitation in upward gaze. With medial wall fractures,
limited abduction due to medial rectus incarceration
may result.
Diagnosis:
CT scanning is highly useful in the assessment of
orbital trauma and associated injures to the brain and
sinuses. Coronal views (direct or reconstructed) should
be requested when orbital trauma is present.
Plain radiographs are not sufficient. They may be
helpful in confirming fractures and in the delineation of
air-fluid levels in the paranasal sinuses, but they may
fail to show the existence and extent of orbital
fractures.
Surgical repair of a fractured orbital wall would be
indicated in the following instances: 1) Significant
enophthalmos. 2) Diplopia in primary gaze or in a
functional gaze. 3) Significant limitation of extraocular
movements.
References:
1. Levin AV. Eye trauma. In: Fleisher GR, Ludwig
S (eds). Textbook of Pediatric Emergency Medicine,
3rd edition. 1993, Baltimore, MD, Williams and
Wilkins, pp. 1200-1209.
2. Mead MD. Evaluation and Initial Management of
Patients with Ocular and Adnexal Trauma. In: Albert
DM, Jakobiec FA (eds). Principles and Practice of
Ophthalmology. 1994, Philadelphia, Saunders, Volume
5, pp. 3362-3375.
3. Friendly DS, Jaafar MS. Ocular Trauma. In:
Eichelberger MR. Pediatric Trauma. 1993, St. Louis,
pp. 401-410.
Return to Radiology Cases In Ped Emerg Med Case Selection Page
Return to Univ. Hawaii Dept. Pediatrics Home Page
 The brain is normal. The CT cut shown is taken in
the axial projection (i.e., the long axis of his body is
perpendicular to the plane of the CT scanner) through
the orbits using a "bone window" contrast setting. The
black arrow points to the medial wall of the left orbit
which is fractured and pushed medially.
Additional coronal CT views are taken of the orbits
by hyperextending his neck so that the long axis of his
head is closer to being parallel with the plane of the CT
scanner. Since axial cuts are parallel with the floor of
the orbit, some fractures of the orbital floor are not well
visualized. By repositioning the patient so that the CT
cuts are perpendicular to the orbital floor, a fracture of
the orbital floor can be more accurately visualized.
View coronal CT cut.
The brain is normal. The CT cut shown is taken in
the axial projection (i.e., the long axis of his body is
perpendicular to the plane of the CT scanner) through
the orbits using a "bone window" contrast setting. The
black arrow points to the medial wall of the left orbit
which is fractured and pushed medially.
Additional coronal CT views are taken of the orbits
by hyperextending his neck so that the long axis of his
head is closer to being parallel with the plane of the CT
scanner. Since axial cuts are parallel with the floor of
the orbit, some fractures of the orbital floor are not well
visualized. By repositioning the patient so that the CT
cuts are perpendicular to the orbital floor, a fracture of
the orbital floor can be more accurately visualized.
View coronal CT cut.
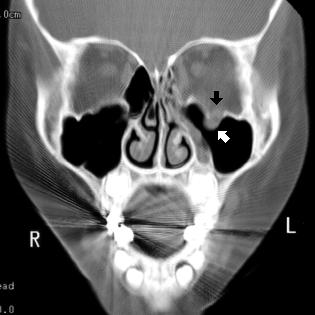 These coronal views reveal a fracture of the left
orbital floor (black arrow). The white arrow points to the
inferior rectus muscle protruding into the maxillary
sinus through the orbital floor fracture site. The clinical
findings suggest that there may be entrapment of the
left inferior rectus muscle, leading to restriction in
upward and downward gaze and diplopia when trying to
look in these directions. The small depressed fracture
of the medial wall of the left orbit with opacification of
the left ethmoid air cells is again visible.
Fractures of the orbital floor may be difficult to
visualize on an axial CT scan through the orbits since
the orbital floor is parallel to the plane of the scan.
Fractures are best seen when the fracture is
perpendicular or oblique to the plane of the scan.
Thus, when an orbital floor fracture is suspected, as in
trauma to the orbit, coronal scans of the orbit should be
obtained, provided that the patient can be positioned
properly.
Orbital wall fractures:
The orbital bones are very delicate and their
thickness is similar to that of an eggshell. Orbital wall
fractures most often occur in the orbital floor and
sometimes in the medial wall, because these are the
weakest regions of the bony orbit. The proximity of the
paranasal sinuses, nerves, vessels, extraocular
muscles, globe and other orbital structures predispose
them to a wide variety of possible damage from injury
producing orbital fractures.
An orbital blow out fracture refers to a fracture of the
orbital floor, usually without involvement of the orbital
rim. The impacting object typically has a diameter that
is larger than that of the orbital opening. Examples
include a fist, tennis ball, baseball, snowball or door
knob. The mechanism of a blow out fracture is
controversial. There are two main theories that are
likely: 1) The fracture results from a sudden increase in
intraorbital pressure when the globe is being pushed
posteriorly. 2) The fracture is the result of "buckling"
forces which are transmitted to the orbital bones by
transient deformity of the orbital rim.
An aide to the evaluation of children with orbital
fractures is the mnemonic HEADER:
Hyphema: Evaluate the child for bleeding in the
anterior chamber and for other intraocular injuries.
Emphysema: Orbital emphysema is due to a
fracture of the medial wall and/or inferior wall which
permits communication between the ethmoid sinus
and/or the maxillary sinus with the orbital contents. In
order to make the diagnosis of orbital emphysema
clinically, the orbit should be palpated for crepitus.
Subcutaneous air can be dramatic when the patient
blows his/her nose. Patients may notice eye swelling
when blowing their nose. Orbital emphysema may be
visible on a plain radiograph of the orbit. It is also
visible on CT scans.
Epistaxis: A fracture of the medial orbital wall can
result in a significant nose bleed.
Anesthesia or hypoaesthesia in the distribution of
the second branch of the trigeminal nerve must be
suspected in any fracture involving the infraorbital
canal. The distribution involves the lower eyelid and
the cheek down to the upper lip on the side of the
injury.
Diplopia: Double vision has essentially two primary
mechanisms: 1) A mechanical entrapment of an eye
muscle, most commonly, the inferior rectus muscle, or
the inferior oblique muscle. 2) A paralytic component
where injury to the third cranial nerve has occurred.
The third cranial nerve innervates both the inferior
rectus and the inferior oblique muscle. Hemorrhage
and edema within the extraocular muscles may also
cause transient paresis.
Exophthalmos is secondary to intraorbital
hemorrhage and edema which pushes the globe
anteriorly. However, a large fracture of the medial
wall or orbital floor may result in enophthalmos.
Restriction: Entrapment of extraocular muscles and
orbital tissue in the fracture site leads to decreased
ocular motility. With orbital floor fractures, the inferior
rectus muscle most commonly is entrapped leading to
limitation in upward gaze. With medial wall fractures,
limited abduction due to medial rectus incarceration
may result.
Diagnosis:
CT scanning is highly useful in the assessment of
orbital trauma and associated injures to the brain and
sinuses. Coronal views (direct or reconstructed) should
be requested when orbital trauma is present.
Plain radiographs are not sufficient. They may be
helpful in confirming fractures and in the delineation of
air-fluid levels in the paranasal sinuses, but they may
fail to show the existence and extent of orbital
fractures.
Surgical repair of a fractured orbital wall would be
indicated in the following instances: 1) Significant
enophthalmos. 2) Diplopia in primary gaze or in a
functional gaze. 3) Significant limitation of extraocular
movements.
References:
1. Levin AV. Eye trauma. In: Fleisher GR, Ludwig
S (eds). Textbook of Pediatric Emergency Medicine,
3rd edition. 1993, Baltimore, MD, Williams and
Wilkins, pp. 1200-1209.
2. Mead MD. Evaluation and Initial Management of
Patients with Ocular and Adnexal Trauma. In: Albert
DM, Jakobiec FA (eds). Principles and Practice of
Ophthalmology. 1994, Philadelphia, Saunders, Volume
5, pp. 3362-3375.
3. Friendly DS, Jaafar MS. Ocular Trauma. In:
Eichelberger MR. Pediatric Trauma. 1993, St. Louis,
pp. 401-410.
These coronal views reveal a fracture of the left
orbital floor (black arrow). The white arrow points to the
inferior rectus muscle protruding into the maxillary
sinus through the orbital floor fracture site. The clinical
findings suggest that there may be entrapment of the
left inferior rectus muscle, leading to restriction in
upward and downward gaze and diplopia when trying to
look in these directions. The small depressed fracture
of the medial wall of the left orbit with opacification of
the left ethmoid air cells is again visible.
Fractures of the orbital floor may be difficult to
visualize on an axial CT scan through the orbits since
the orbital floor is parallel to the plane of the scan.
Fractures are best seen when the fracture is
perpendicular or oblique to the plane of the scan.
Thus, when an orbital floor fracture is suspected, as in
trauma to the orbit, coronal scans of the orbit should be
obtained, provided that the patient can be positioned
properly.
Orbital wall fractures:
The orbital bones are very delicate and their
thickness is similar to that of an eggshell. Orbital wall
fractures most often occur in the orbital floor and
sometimes in the medial wall, because these are the
weakest regions of the bony orbit. The proximity of the
paranasal sinuses, nerves, vessels, extraocular
muscles, globe and other orbital structures predispose
them to a wide variety of possible damage from injury
producing orbital fractures.
An orbital blow out fracture refers to a fracture of the
orbital floor, usually without involvement of the orbital
rim. The impacting object typically has a diameter that
is larger than that of the orbital opening. Examples
include a fist, tennis ball, baseball, snowball or door
knob. The mechanism of a blow out fracture is
controversial. There are two main theories that are
likely: 1) The fracture results from a sudden increase in
intraorbital pressure when the globe is being pushed
posteriorly. 2) The fracture is the result of "buckling"
forces which are transmitted to the orbital bones by
transient deformity of the orbital rim.
An aide to the evaluation of children with orbital
fractures is the mnemonic HEADER:
Hyphema: Evaluate the child for bleeding in the
anterior chamber and for other intraocular injuries.
Emphysema: Orbital emphysema is due to a
fracture of the medial wall and/or inferior wall which
permits communication between the ethmoid sinus
and/or the maxillary sinus with the orbital contents. In
order to make the diagnosis of orbital emphysema
clinically, the orbit should be palpated for crepitus.
Subcutaneous air can be dramatic when the patient
blows his/her nose. Patients may notice eye swelling
when blowing their nose. Orbital emphysema may be
visible on a plain radiograph of the orbit. It is also
visible on CT scans.
Epistaxis: A fracture of the medial orbital wall can
result in a significant nose bleed.
Anesthesia or hypoaesthesia in the distribution of
the second branch of the trigeminal nerve must be
suspected in any fracture involving the infraorbital
canal. The distribution involves the lower eyelid and
the cheek down to the upper lip on the side of the
injury.
Diplopia: Double vision has essentially two primary
mechanisms: 1) A mechanical entrapment of an eye
muscle, most commonly, the inferior rectus muscle, or
the inferior oblique muscle. 2) A paralytic component
where injury to the third cranial nerve has occurred.
The third cranial nerve innervates both the inferior
rectus and the inferior oblique muscle. Hemorrhage
and edema within the extraocular muscles may also
cause transient paresis.
Exophthalmos is secondary to intraorbital
hemorrhage and edema which pushes the globe
anteriorly. However, a large fracture of the medial
wall or orbital floor may result in enophthalmos.
Restriction: Entrapment of extraocular muscles and
orbital tissue in the fracture site leads to decreased
ocular motility. With orbital floor fractures, the inferior
rectus muscle most commonly is entrapped leading to
limitation in upward gaze. With medial wall fractures,
limited abduction due to medial rectus incarceration
may result.
Diagnosis:
CT scanning is highly useful in the assessment of
orbital trauma and associated injures to the brain and
sinuses. Coronal views (direct or reconstructed) should
be requested when orbital trauma is present.
Plain radiographs are not sufficient. They may be
helpful in confirming fractures and in the delineation of
air-fluid levels in the paranasal sinuses, but they may
fail to show the existence and extent of orbital
fractures.
Surgical repair of a fractured orbital wall would be
indicated in the following instances: 1) Significant
enophthalmos. 2) Diplopia in primary gaze or in a
functional gaze. 3) Significant limitation of extraocular
movements.
References:
1. Levin AV. Eye trauma. In: Fleisher GR, Ludwig
S (eds). Textbook of Pediatric Emergency Medicine,
3rd edition. 1993, Baltimore, MD, Williams and
Wilkins, pp. 1200-1209.
2. Mead MD. Evaluation and Initial Management of
Patients with Ocular and Adnexal Trauma. In: Albert
DM, Jakobiec FA (eds). Principles and Practice of
Ophthalmology. 1994, Philadelphia, Saunders, Volume
5, pp. 3362-3375.
3. Friendly DS, Jaafar MS. Ocular Trauma. In:
Eichelberger MR. Pediatric Trauma. 1993, St. Louis,
pp. 401-410.